Complex Bicondylar Tibial Plateau Fracture with Valgus Collapse and Infection
Score and Comment on this Case
Clinical Details
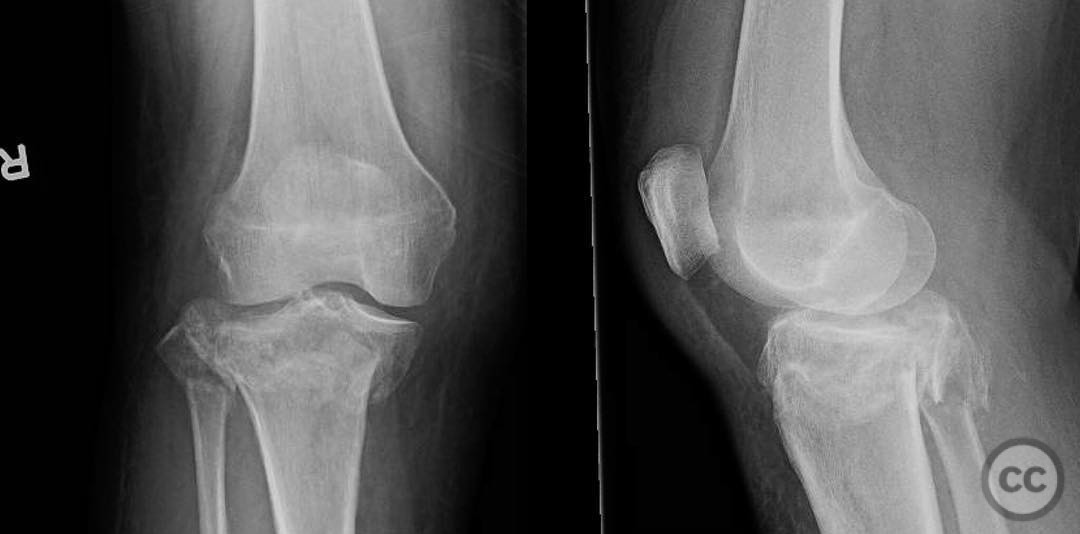
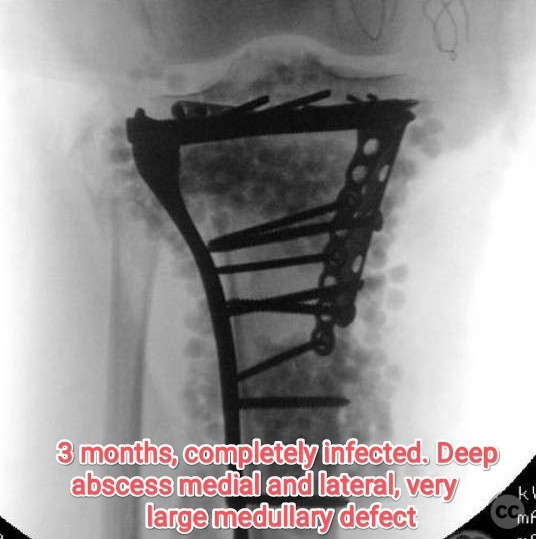
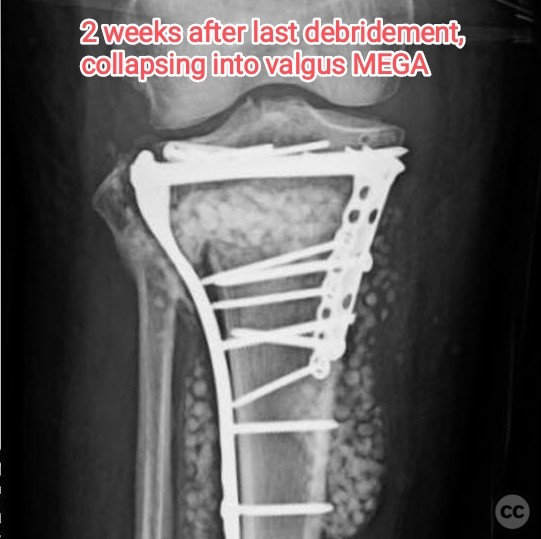
Clinical and radiological findings: A 62-year-old female patient sustained a fall from a log, resulting in a complex bicondylar tibial plateau fracture. Initial radiographs were obtained prior to the application of an external fixator, while a computed tomography (CT) scan was performed post-external fixation. The medial plateau demonstrated satisfactory reduction with the external fixator, and the joint surface appeared relatively preserved. However, subsequent imaging revealed progressive valgus collapse over time. At 6 weeks post-injury, there was noted valgus deformity, which worsened by 3 months post-injury, accompanied by deep infection and large medullary defects on both the medial and lateral aspects. The joint had healed, but the metaphysis remained unhealed. Cultures grew Methicillin-Sensitive Staphylococcus Aureus (MSSA).
Preoperative Plan
Planning remarks: The preoperative plan involved addressing the lateral plateau, likely through a lateral approach, given the noted reduction of the medial side with external fixation. The aim was to achieve anatomical reduction and stable fixation of the lateral plateau to prevent further valgus collapse.
Surgical Discussion
Patient positioning: Supine positioning was utilized, with the affected limb placed on a radiolucent table to facilitate intraoperative fluoroscopic imaging.
Anatomical surgical approach: A lateral parapatellar approach was employed to access the lateral tibial plateau. This involved an incision along the lateral aspect of the knee, followed by careful dissection to expose the lateral condyle. Subperiosteal elevation was performed to visualize the fracture site and facilitate reduction and fixation.
Operative remarks:Intraoperative findings indicated that the lateral plateau was fixed slightly lower than optimal, contributing to subsequent valgus collapse. Despite initial satisfactory reduction, progressive valgus deformity developed over time, complicated by deep infection and significant bone loss in the metaphysis. Multiple debridements were necessary to manage the infection, which cultured MSSA. The presence of a large medullary defect posed a challenge for metaphyseal healing.
Postoperative protocol: Postoperative rehabilitation was initially limited due to infection management and instability concerns. Weight-bearing status was likely restricted until infection control and adequate fracture healing were achieved.
Follow up: Not specified
Orthopaedic implants used: External fixator, internal fixation hardware (specific implants not detailed).
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities



Article viewed 143 times
26 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Complex Bicondylar Tibial Plateau Fracture with Valgus Collapse and Infection. Journal of Orthopaedic Surgery and Traumatology. Case Report 8017676 Published Online Jul 26 2025.