Complex Bilateral Pelvic Ring Injury: Posterior Sacral ORIF and Anterior Symphyseal Fixation
Score and Comment on this Case
Clinical Details
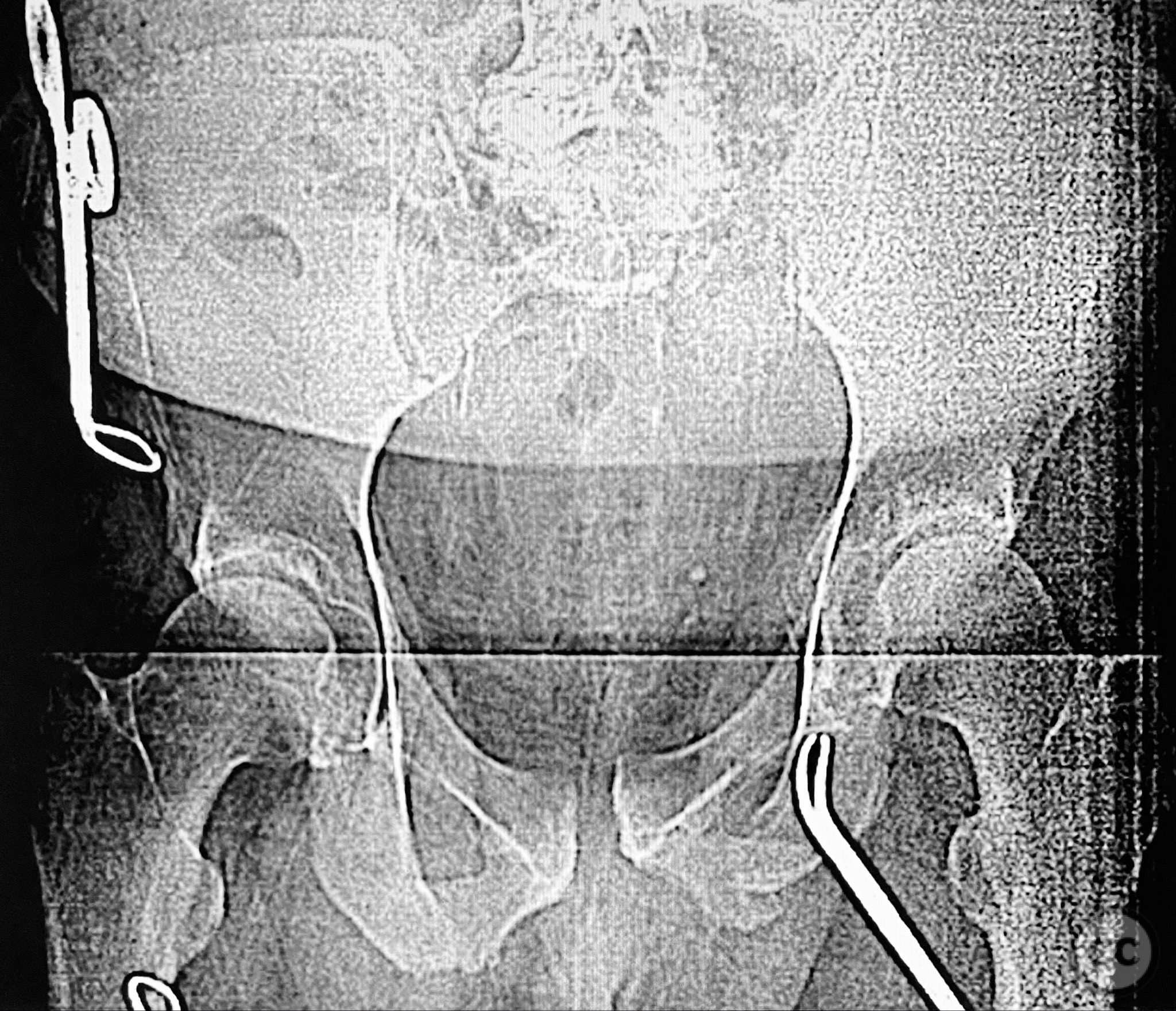
Clinical and radiological findings: Middle-aged male with a high-energy pelvic ring injury, presenting with significant pain and mechanical instability. Initial radiographs demonstrated comminution and displacement of the posterior pelvic ring, including sacral fractures and disruption of the anterior ring at the pubic symphysis and rami. Application of a circumferential pelvic sheet provided partial reduction and improved comfort. No neurovascular deficits were noted. CT imaging confirmed a comminuted sacral fracture (AO/OTA 61-C1.3), with bilateral pubic rami fractures and symphyseal diastasis. The posterior elements demonstrated both vertical and rotational instability.
Preoperative Plan
Planning remarks: The preoperative plan involved staged management: initial prone positioning for open reduction and internal fixation (ORIF) of the sacrum, utilizing the dorsal cortical fracture edges for direct reduction and clamping, followed by percutaneous iliosacral screw fixation and a posterior transiliac screw. Definitive anterior ring stabilization was planned subsequently via open reduction and internal fixation of the symphysis and pubic rami through an anterior approach.
Surgical Discussion
Patient positioning: Prone positioning on a radiolucent table for posterior pelvic ring fixation, followed by supine positioning for anterior ring stabilization.
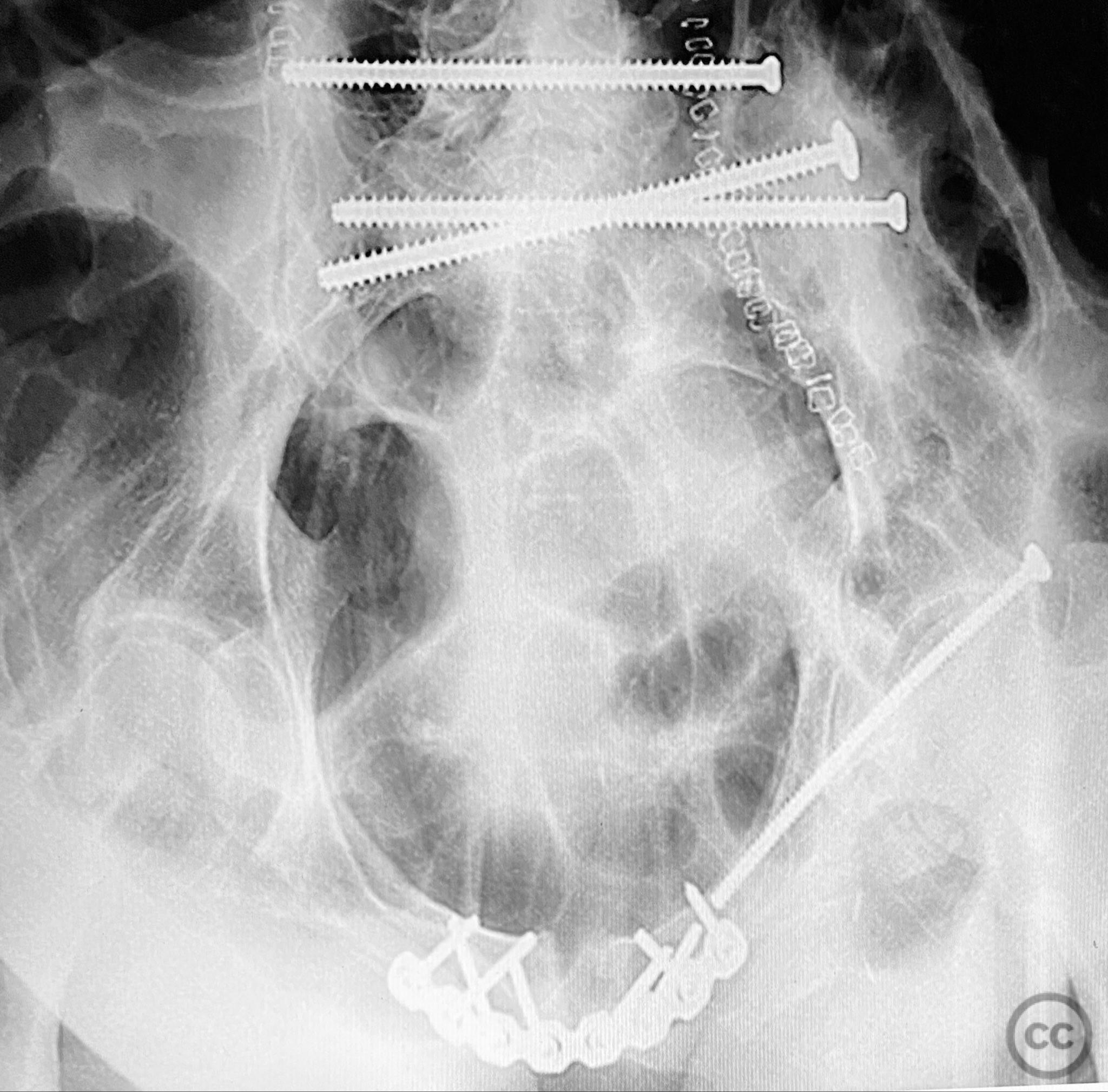
Anatomical surgical approach: Posterior approach to the sacrum via a midline longitudinal incision, subperiosteal dissection to expose the dorsal sacral cortex and fracture lines. Direct reduction of the sacral fragments using clamps applied to the dorsal cortical edges, with intraoperative fluoroscopic guidance. Placement of iliosacral screws (non-cannulated, <130mm length due to implant availability at the time) across S1, supplemented by a posterior transiliac screw. For anterior fixation, a Pfannenstiel incision was used to expose the symphysis pubis and superior pubic rami; reduction achieved with pointed reduction forceps, followed by plate osteosynthesis of the symphysis and screw fixation of the rami as indicated.
Operative remarks:The staged approach allowed direct assessment and refinement of posterior reduction using dorsal cortical landmarks, which was critical given the comminution and displacement pattern. The absence of long cannulated screws limited optimal iliosacral screw placement; screws were contained within the osseous fixation pathway but not ideally positioned for maximal safety or precision by contemporary standards. Anterior ring stabilization was performed after confirming satisfactory posterior reduction on postoperative CT. The sequence addressed both vertical and rotational instability, but implant limitations may have increased risk for suboptimal fixation or neurovascular compromise. In current practice, advanced imaging, navigation, and longer cannulated screws would be utilized to optimize screw trajectory and safety.
Postoperative protocol: Early mobilization with protected weight bearing for 8-12 weeks, depending on radiographic evidence of healing and clinical stability. Thromboprophylaxis until full mobilization. Progressive physiotherapy focusing on core stability and hip range of motion.
Follow up: Not specified
Orthopaedic implants used: 6.5mm non-cannulated iliosacral screws (<130mm), posterior transiliac screw, anterior symphyseal plate, cortical screws for pubic rami
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities








Article viewed 147 times
12 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Complex Bilateral Pelvic Ring Injury: Posterior Sacral ORIF and Anterior Symphyseal Fixation. Journal of Orthopaedic Surgery and Traumatology. Case Report 7634064 Published Online Sep 12 2025.