Complex Open Tibia Fracture with Proximal Tibiofibular Joint Dislocation and Compartment Syndrome.
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: A 34-year-old male sustained a high-energy injury from a motorcycle collision, resulting in a 3b open tibia fracture with medial, posteromedial, and lateral exposure. Radiographs and clinical examination revealed a severe skeletal injury characterized by a tibia and fibula fracture, complete disruption of the proximal tibiofibular interosseous membrane, and dislocation of the proximal tibiofibular joint. The patient developed compartment syndrome necessitating four-compartment fasciotomies.
Preoperative Plan
Planning remarks: The preoperative plan included early definitive care with intramedullary (IM) nailing of the tibia and fibula for skeletal stabilization to facilitate soft tissue management. Fasciotomy was performed to address compartment syndrome, followed by wound vacuum-assisted closure (VAC) therapy. Subsequent soft tissue coverage was planned with rotational muscle flap and skin grafting.
Surgical Discussion
Patient positioning: Supine positioning on a radiolucent table to facilitate access for intramedullary nailing and fasciotomy.
Anatomical surgical approach: Anteromedial approach to the tibia for intramedullary nailing, with additional incisions for fasciotomy along the anterior, lateral, and posterior compartments of the leg. The proximal fibula was addressed through a lateral approach for IM nailing.
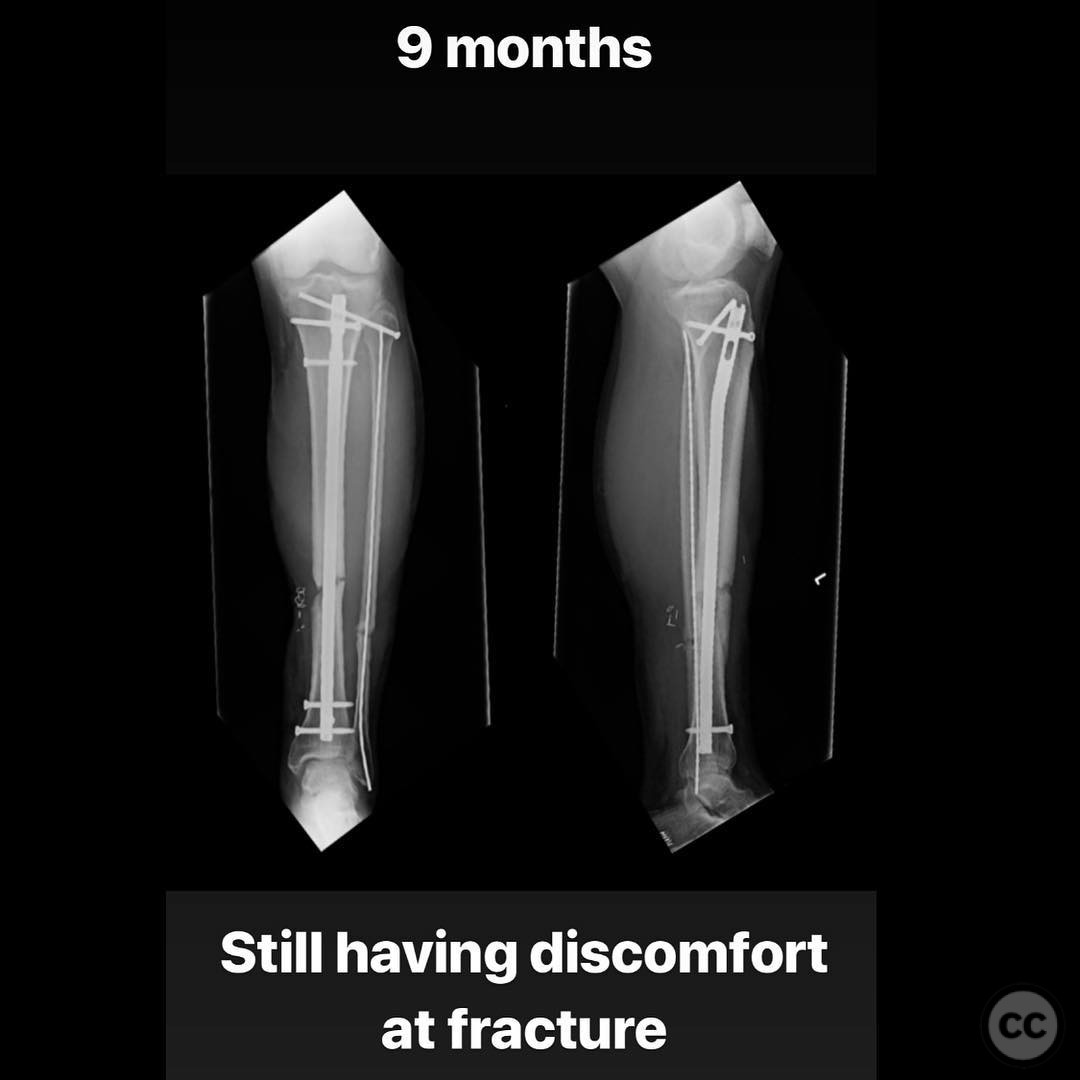
Operative remarks:The initial surgical intervention focused on stabilizing the fracture and managing the soft tissue injury with VAC therapy and planned flap coverage. At 9 months post-injury, the patient presented with septic nonunion characterized by intermittent serous drainage at the fracture site. Laboratory workup confirmed infection with MSSA. Treatment involved removal of the tibial nail, reaming with cultures taken from reamings, insertion of an antibiotic-coated nail using PMMA mixed with vancomycin and tobramycin, and systemic antibiotics targeting MSSA. Once infection markers normalized, exchange nailing was performed.
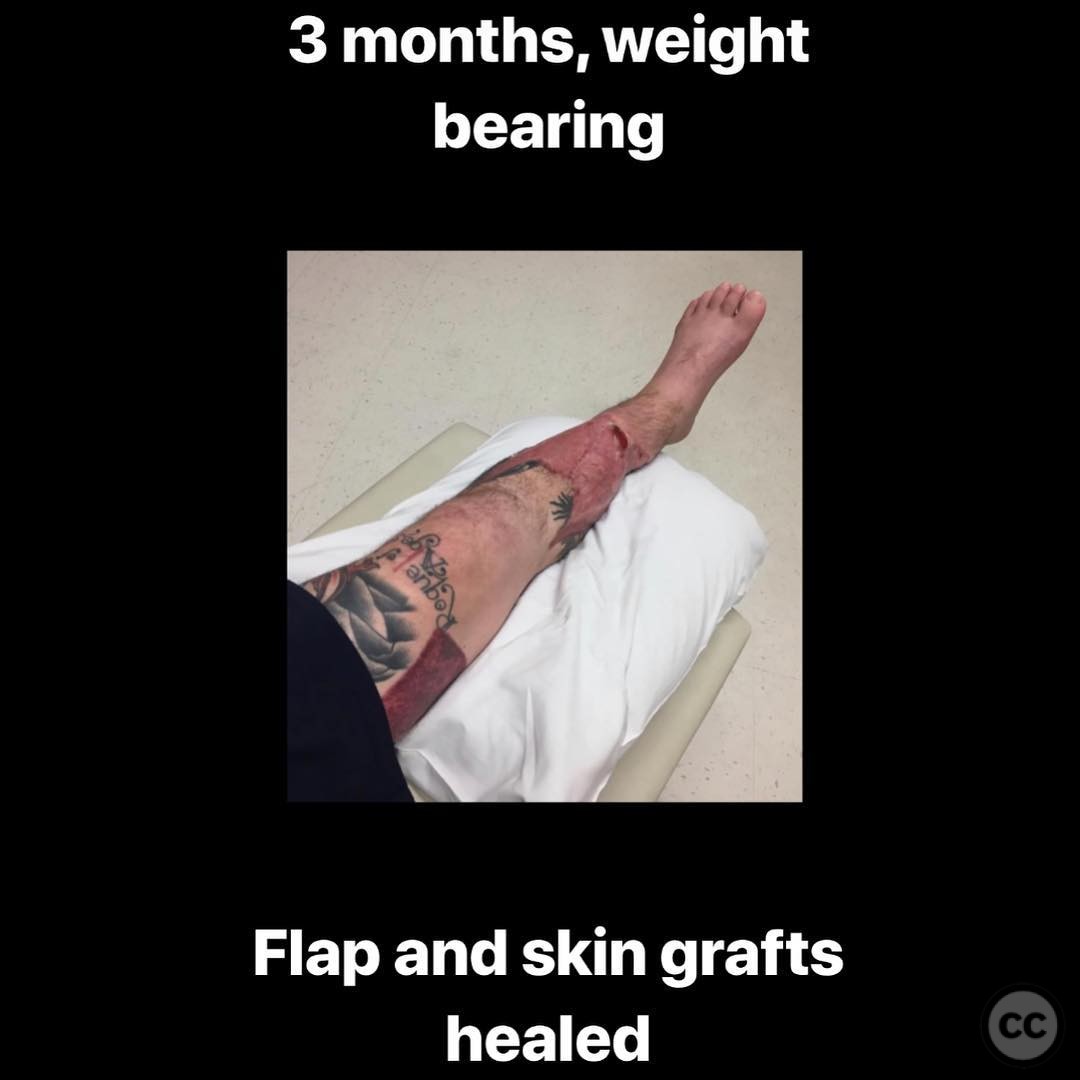
Postoperative protocol: Initial non-weight bearing status postoperatively, progressing to weight bearing as tolerated at 3 months once soft tissue healing was confirmed. Following antibiotic nail insertion, weight bearing was allowed to promote dynamization and healing around the nail.
Orthopaedic implants used: Intramedullary nails for tibia and fibula, wound VAC system, PMMA antibiotic-coated nail (vancomycin and tobramycin). Technique for abx nail if you’ve never done it. 1) 40 French chest tube, mineral oil. 2) threaded ilizarov rod and eyelet 3) table top bender 4) pmma and Vanc/tobra . . . Measure and cut ilizarov rod to length, anticipating the herzog bend and eyelet. Cut chest tube to a little longer length, lube up the inside w mineral oil. Place rod into tube. Mix 4g vanc, 2.4g tobra w 40g pmma. Inject cement into chest tube slowly. Allow to harden (be patient!). Cut chest tube off nail w 10blade. Enjoy your creation!!! . . . Depending on the nonunion’s stability, you can let the patient weight bear on the abx nail- often they will heal around it. If highly unstable, add an ex-fix.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities






. T_2.jpg)
. T_1.jpg)
. Th(.jpg)








Article viewed 174 times
21 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Complex Open Tibia Fracture with Proximal Tibiofibular Joint Dislocation and Compartment Syndrome.. Journal of Orthopaedic Surgery and Traumatology. Case Report 7467635 Published Online Jul 21 2025.