Bilateral Proximal Humerus Fracture Dislocations with Vascular and Neurological Complications.
Score and Comment on this Case
Clinical Details
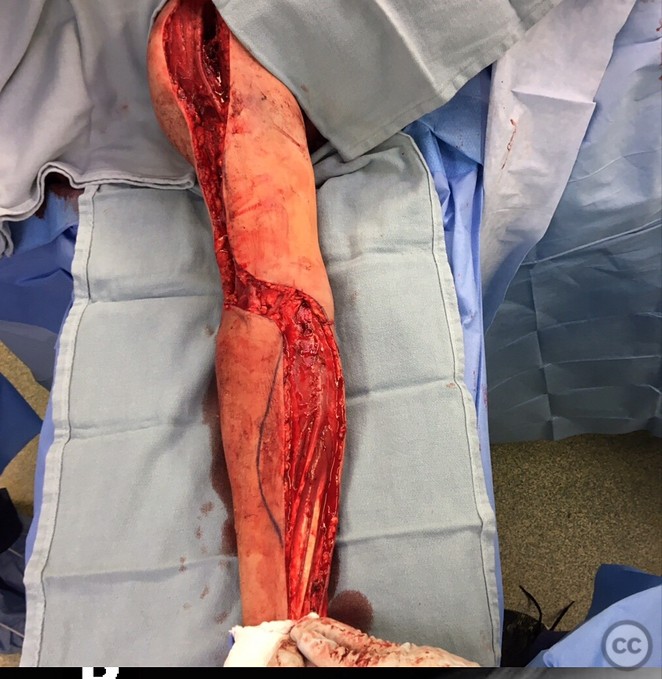
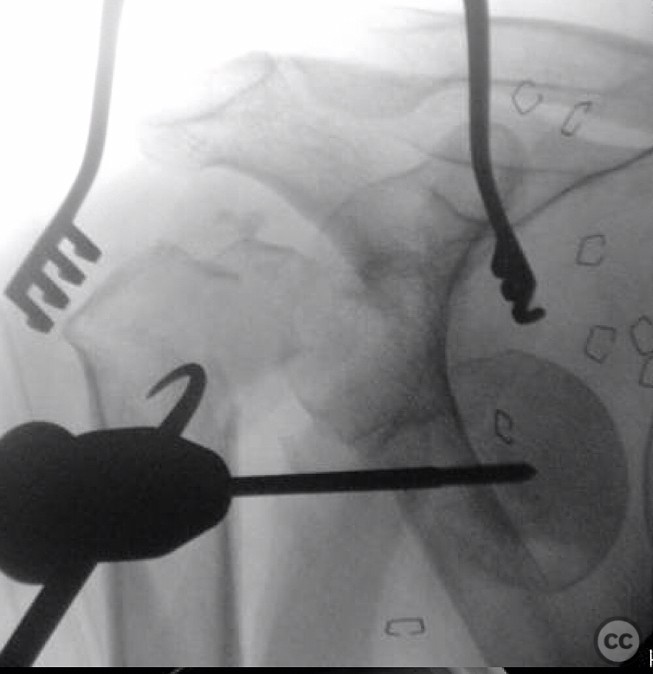
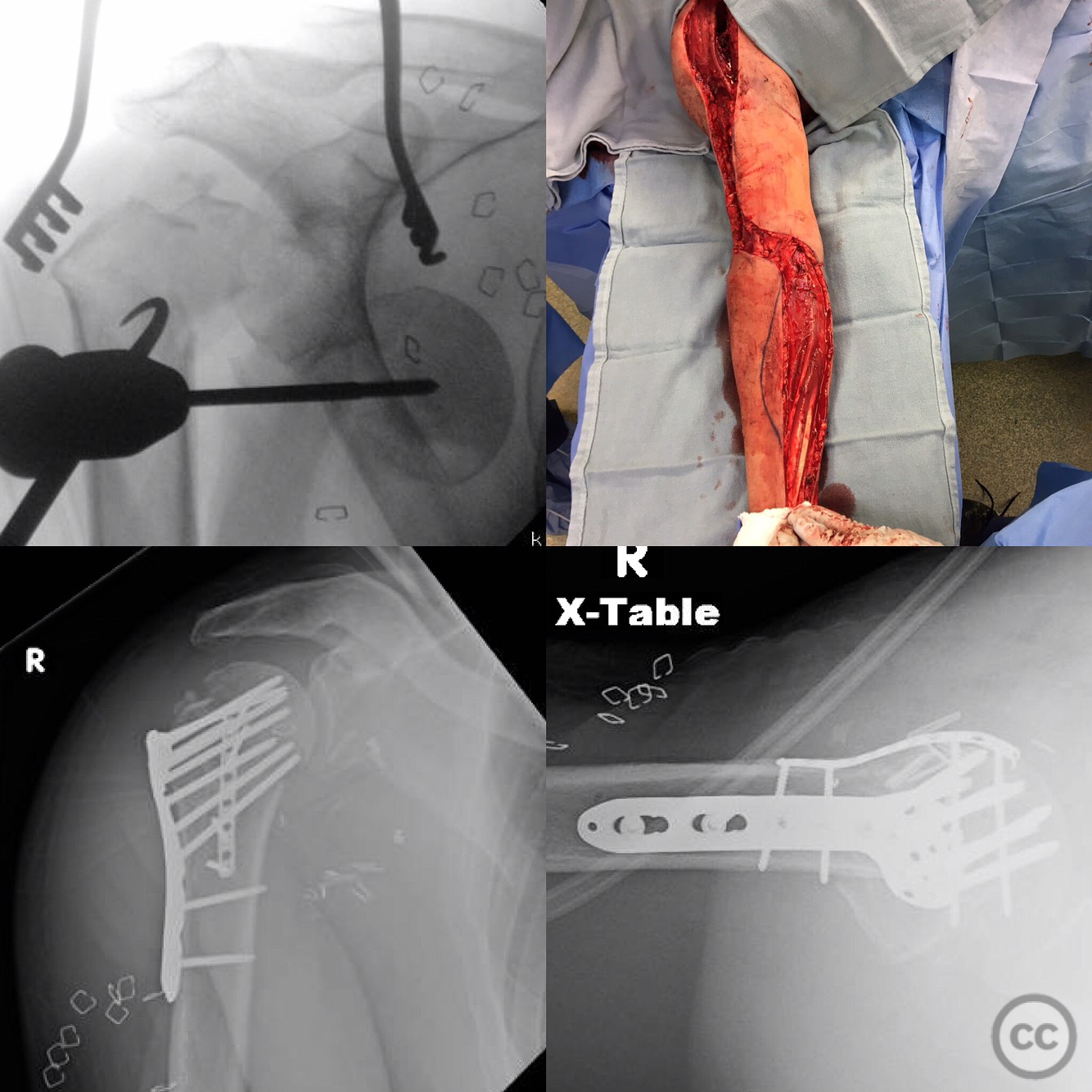
Clinical and radiological findings: A 44-year-old male sustained bilateral proximal humerus fracture dislocations after deflecting a 400lb crate falling from overhead. Radiographs confirmed the presence of bilateral four-part proximal humerus fractures. The right shoulder was associated with a complete brachial plexopathy, axillary artery laceration, axillary vein laceration, and multiple large axillary vein tributary lacerations. There was a 12-hour delay to the operating room. The humeral head on the right side tamponaded the axillary artery at the level of the laceration, preventing further hemorrhage despite the arm being disvascular.
Preoperative Plan
Planning remarks: The preoperative plan included extraction of the humeral head, repair of the axillary artery, ligation of multiple venous injuries, fasciotomies of all compartments, and open reduction and internal fixation (ORIF) of the four-part proximal humerus fracture. The surgical approach was anticipated to be an extended deltopectoral approach for adequate exposure of the vascular structures and fracture site.
Surgical Discussion
Patient positioning: Supine position with the affected arm abducted and externally rotated on a radiolucent table to facilitate surgical access to the shoulder and axillary region.
Anatomical surgical approach: An extended deltopectoral approach was utilized, involving an incision from the coracoid process extending distally along the deltopectoral groove. The cephalic vein was retracted laterally, and subdeltoid dissection was performed to expose the proximal humerus and axillary neurovascular structures. Fasciotomies were performed in all compartments to address potential compartment syndrome.
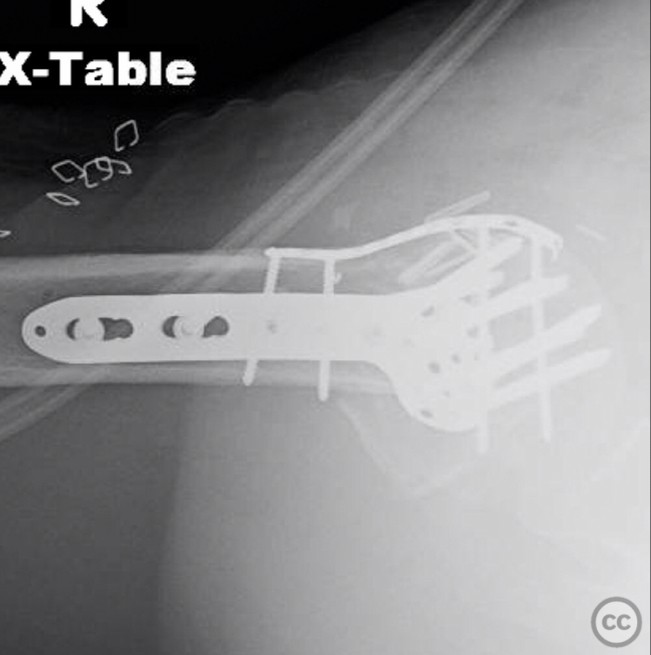
Operative remarks:Significant intraoperative blood loss was encountered, estimated at 5 liters. Despite vascular surgery presence, extensive transfusion was required, including 8 units of packed red blood cells, 8 units of fresh frozen plasma, 1 six-pack of platelets, and 12 liters of crystalloid solution. The humeral head was extracted to allow for axillary artery repair and ligation of venous injuries. ORIF of the proximal humerus fracture was completed using appropriate fixation devices.
Postoperative protocol: Postoperative rehabilitation included immobilization in a shoulder immobilizer initially, with gradual passive range of motion exercises introduced at 2 weeks post-surgery. Active-assisted range of motion exercises were initiated at 6 weeks, progressing to strengthening exercises by 12 weeks postoperatively.
Follow up: Not specified.
Orthopaedic implants used: Locking proximal humerus plate, vascular repair sutures, fasciotomy closure materials.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities


Article viewed 162 times
26 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Bilateral Proximal Humerus Fracture Dislocations with Vascular and Neurological Complications.. Journal of Orthopaedic Surgery and Traumatology. Case Report 47360575 Published Online Jul 26 2025.