Pronation Abduction Ankle Injury with Talar Neck and Lateral Body Fracture.
Score and Comment on this Case
Clinical Details
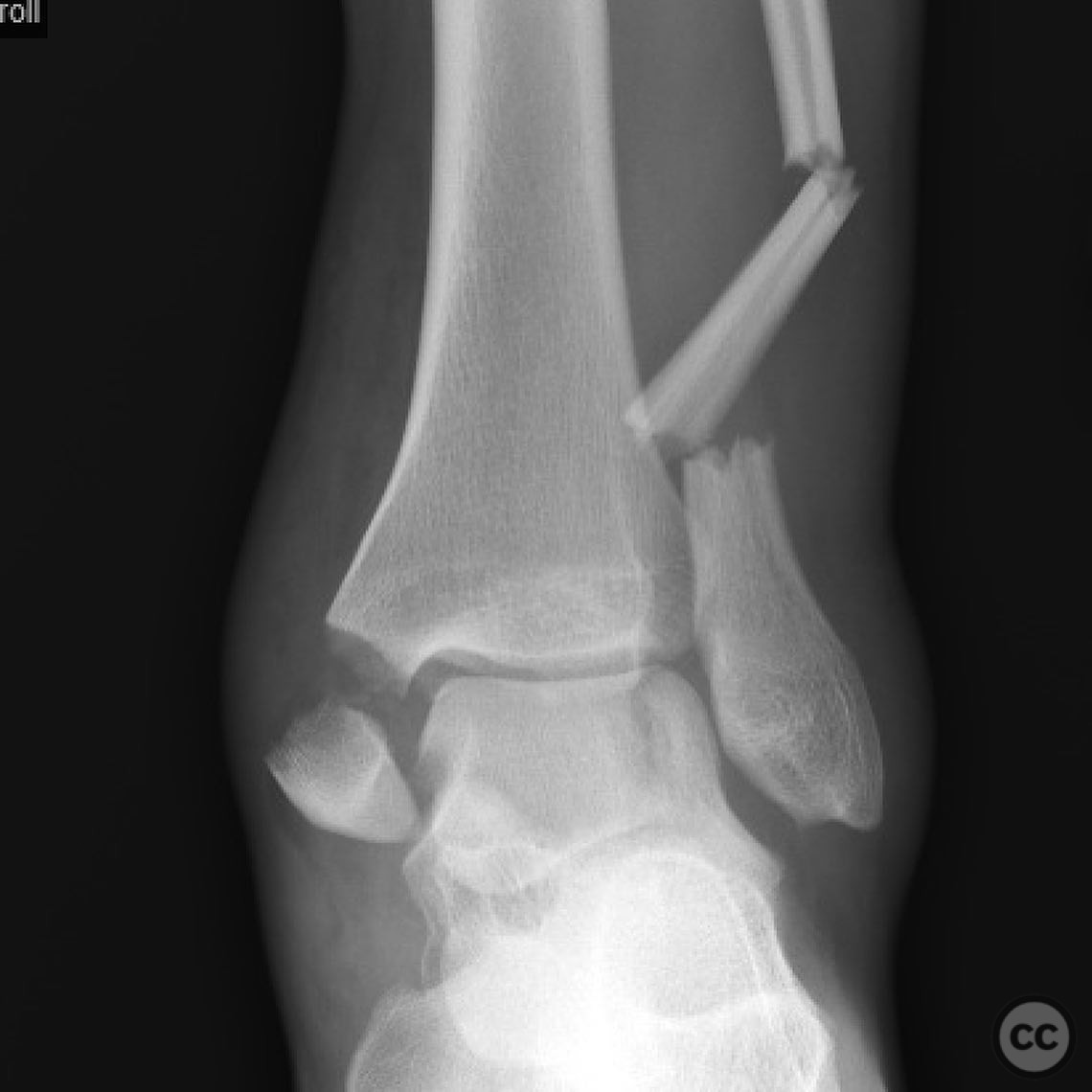
Clinical and radiological findings: A 22-year-old male presented to the emergency department following a fall while rock climbing. The patient sustained a closed injury with some rib fractures but was otherwise isolated. The foot was moderately swollen, and there was evidence of tibial nerve neuropraxia. Dopplerable posterior tibial (PT) and dorsalis pedis (DP) pulses were present. Radiological assessment revealed a pronation abduction injury to the ankle, characterized by a fibular fracture due to bending force, a medial malleolus fracture due to tension failure, and syndesmotic disruption. Additionally, the talus exhibited a neck fracture and a lateral talar body sagittal plane fracture due to hyperdorsiflexion and shearing forces during the dislocation event. The talar injury was classified as a Hawkins Type 1-2a fracture.
Preoperative Plan
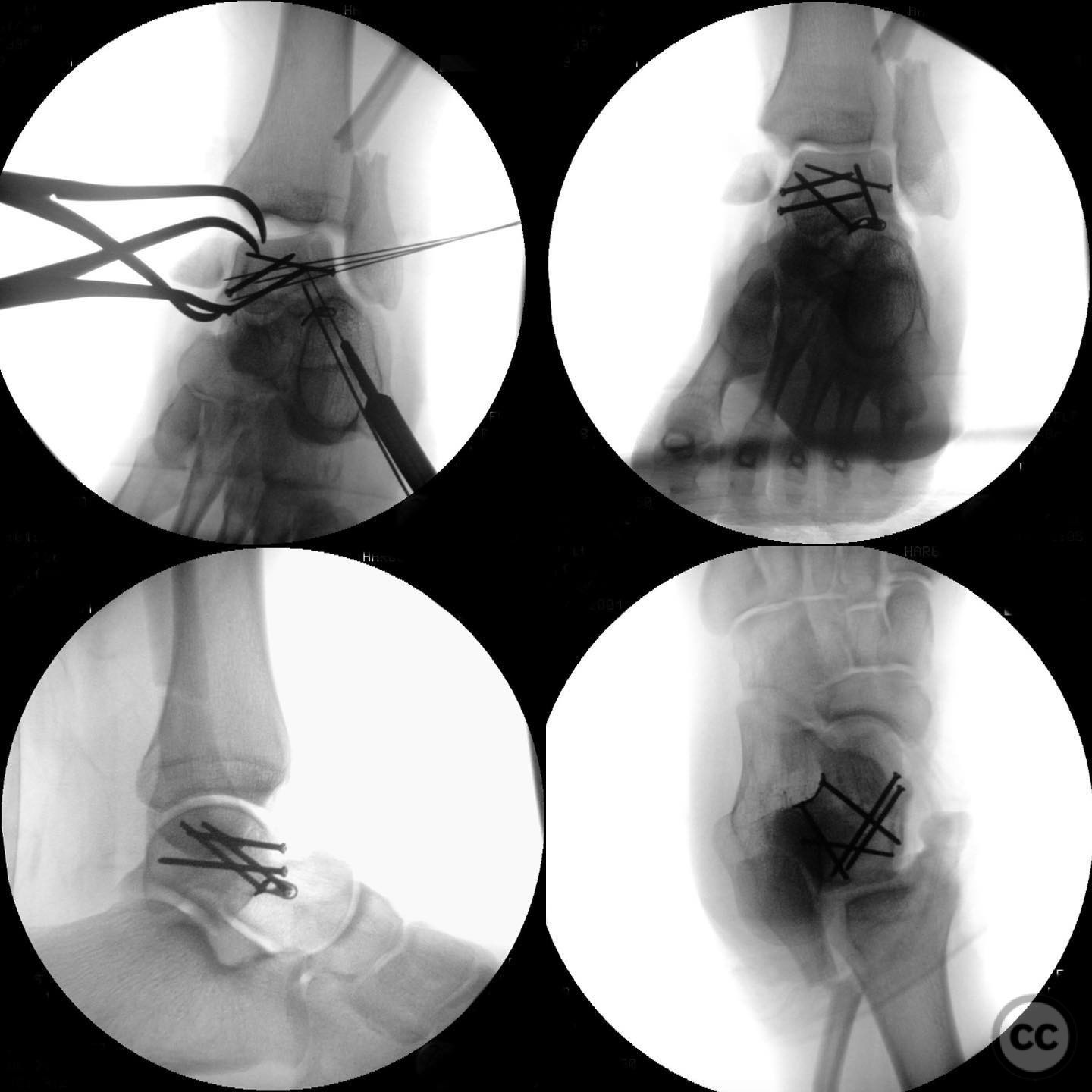
Planning remarks: The preoperative plan involved addressing the talar fractures first, utilizing the medial malleolus fracture and syndesmotic injuries as osteotomies for enhanced exposure. A dorsolateral and dorsomedial approach was planned for the talus. Following talar fixation, attention would be directed towards the ankle and syndesmosis.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table.
Anatomical surgical approach: A dorsolateral approach was made to access the lateral aspect of the talus, followed by a dorsomedial approach for the medial aspect. The medial malleolus fracture was used as an osteotomy site for improved visualization and access to the talar neck and body fractures.
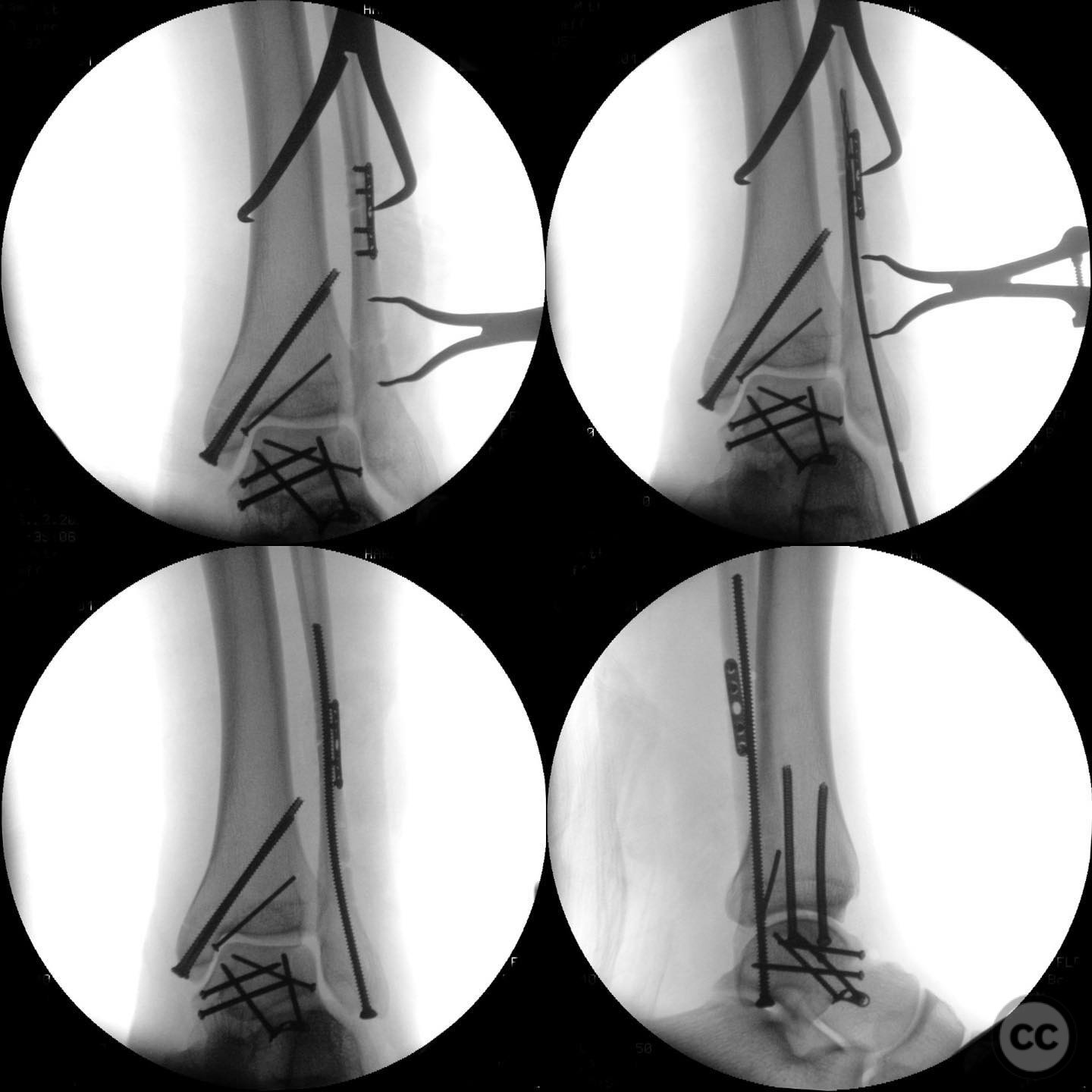
Operative remarks:The surgeon noted that the fibular fracture pattern was unique and particularly suitable for intramedullary (IM) fixation. However, open reduction was necessary to ensure proper alignment and rotational correction. For the syndesmosis, an open reduction was performed, followed by fluoroscopic comparison with the contralateral side, and an O-arm spin was utilized if further confirmation was needed.
Postoperative protocol: Postoperatively, the patient was placed in a non-weight-bearing status for 6 weeks, followed by progressive weight-bearing as tolerated. Range of motion exercises were initiated early to prevent stiffness.
Follow up: Not specified.
Orthopaedic implants used: Intramedullary fibular nail, syndesmotic screws or fixation device (specific type not specified).
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities













Article viewed 197 times
13 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Pronation Abduction Ankle Injury with Talar Neck and Lateral Body Fracture.. Journal of Orthopaedic Surgery and Traumatology. Case Report 46838806 Published Online Jul 13 2025.