Proximal Humerus Fracture Dislocation with Greater Tuberosity Involvement
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: A 32-year-old male sustained a proximal humerus fracture dislocation after falling 20 feet from a tree. The patient presented with a Glasgow Coma Scale of 3, necessitating intubation and emergent craniotomy for a hemopneumothorax and high intracranial pressures. Initial orthopaedic examination revealed no open fractures, bounding radial pulses, and an indeterminate neurological status due to the patient's critical condition. Radiological assessment was deferred until stabilization of intracranial pressures.
Preoperative Plan
Planning remarks: The preoperative plan involved an extended deltopectoral approach to facilitate reduction and fixation of the proximal humerus fracture dislocation. A biceps tenotomy was planned to aid in reduction, with consideration for coracoid osteotomy if vascular injury was suspected.
Surgical Discussion
Patient positioning: The patient was positioned supine with the head of the bed elevated to 45 degrees to accommodate ongoing intracranial pressure management.
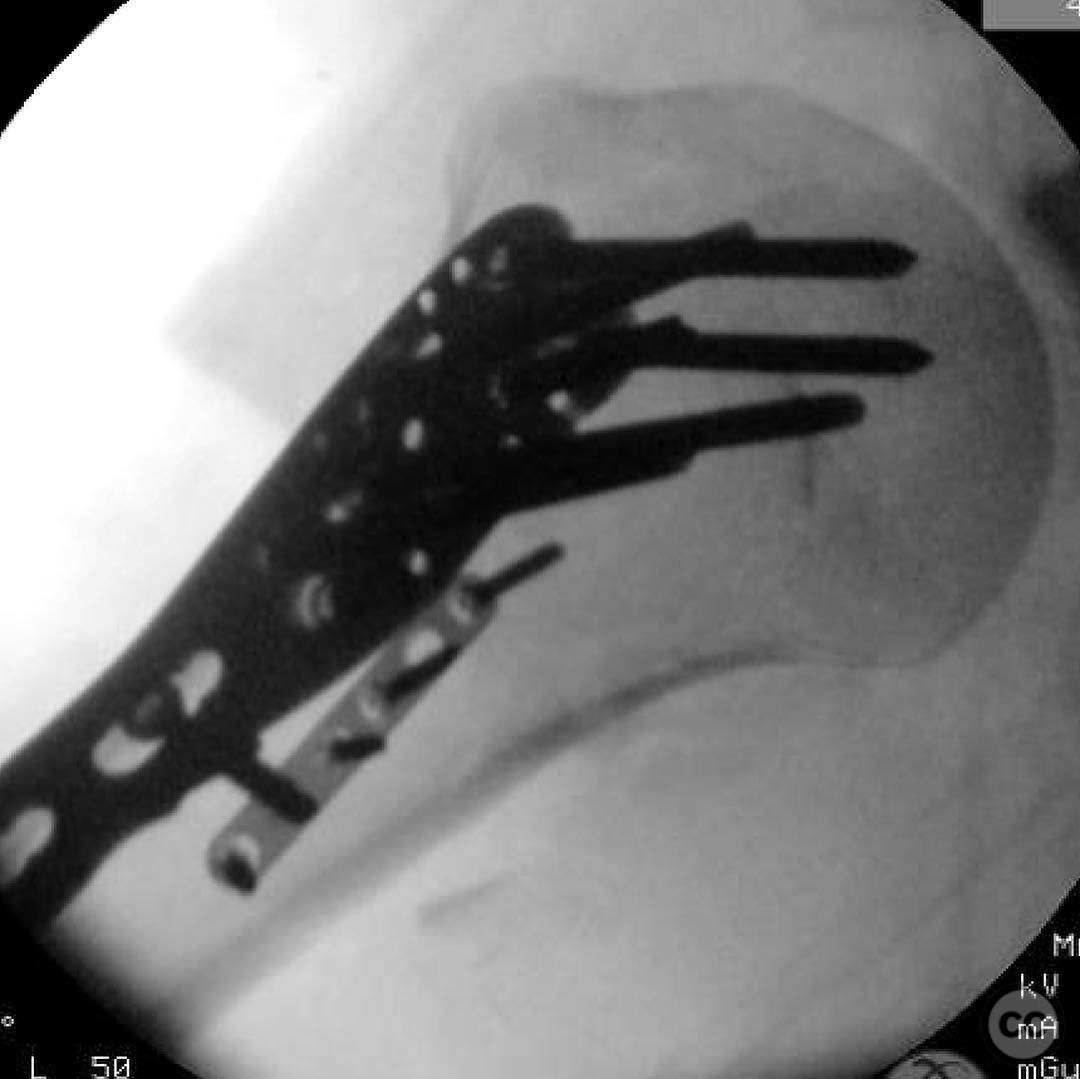
Anatomical surgical approach: The surgical approach utilized an extended deltopectoral incision. A biceps tenotomy was performed to facilitate reduction of the humeral head into the glenoid. A Schanz pin was carefully placed into the calcar or humeral head, with manual protection of the axillary artery and vein during insertion. Following reduction, direct anatomic reduction of the fracture was achieved with interfragmentary compression using 2.7mm lag screws. The greater tuberosity was reduced using sutures in the rotator cuff, held in place with wires, and potentially mini fragment fixation if the fragment size permitted. A laterally based locking plate was applied, ensuring all screws were safely positioned, and cuff sutures were tied to the plate. Biceps tenodesis was performed.
Operative remarks:The surgeon noted the importance of careful placement of the Schanz pin to avoid vascular injury and emphasized the necessity of achieving anatomic reduction to minimize the risk of avascular necrosis (AVN). The use of sutures and wires for greater tuberosity fixation was highlighted as a critical step in restoring native anatomy.
Postoperative protocol: Postoperative rehabilitation included immobilization in a sling with passive range of motion exercises initiated as tolerated, progressing to active-assisted and active range of motion exercises over several weeks. Weight-bearing restrictions were maintained until radiographic evidence of healing.
Follow up: Not specified.
Orthopaedic implants used: Laterally based locking plate, 2.7mm lag screws, Schanz pin, sutures for rotator cuff fixation, wires for greater tuberosity fixation.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities








Article viewed 168 times
23 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Proximal Humerus Fracture Dislocation with Greater Tuberosity Involvement. Journal of Orthopaedic Surgery and Traumatology. Case Report 46063920 Published Online Jul 23 2025.