Vancouver B2 Periprosthetic Femur Fracture in a High-Risk Patient
Score and Comment on this Case
Clinical Details
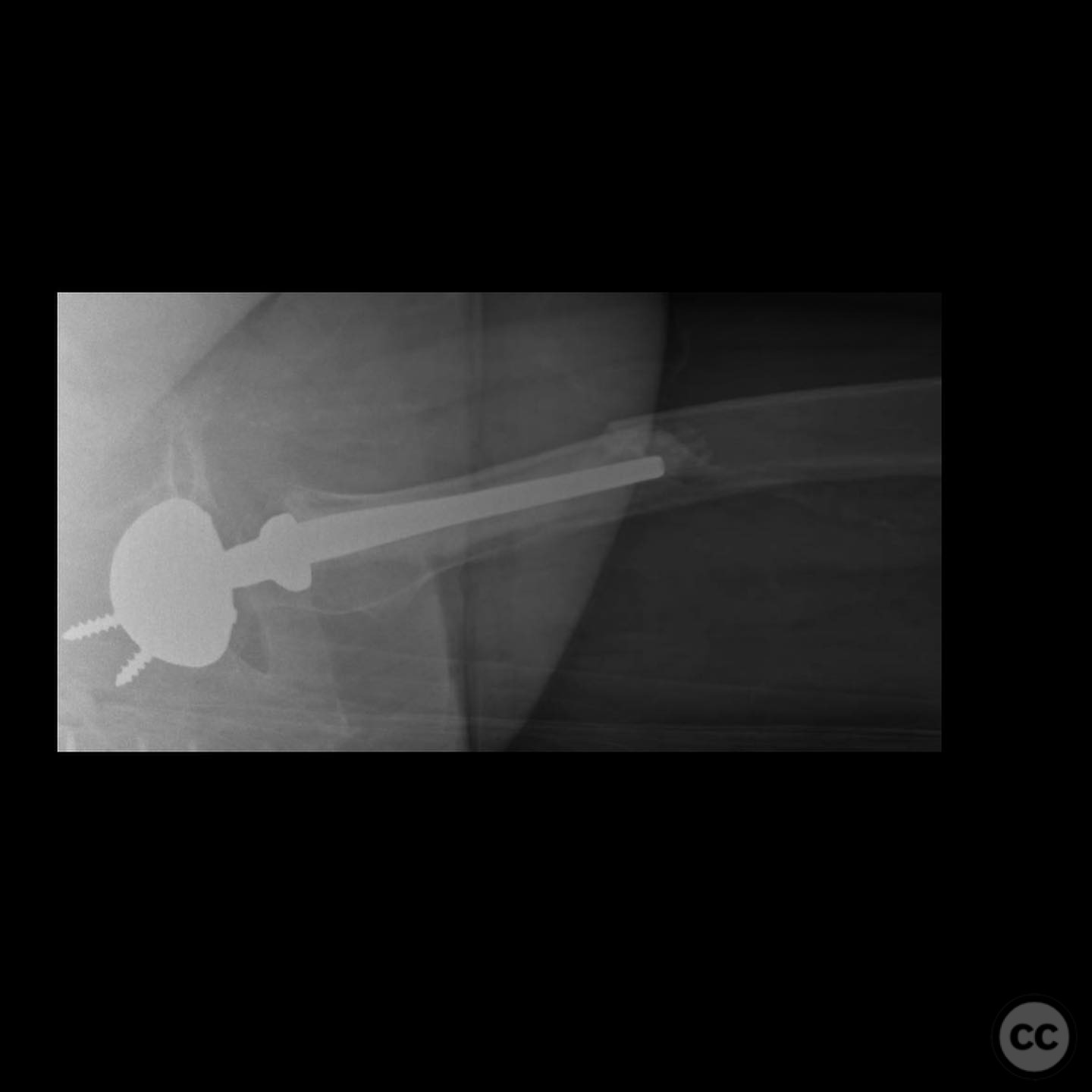
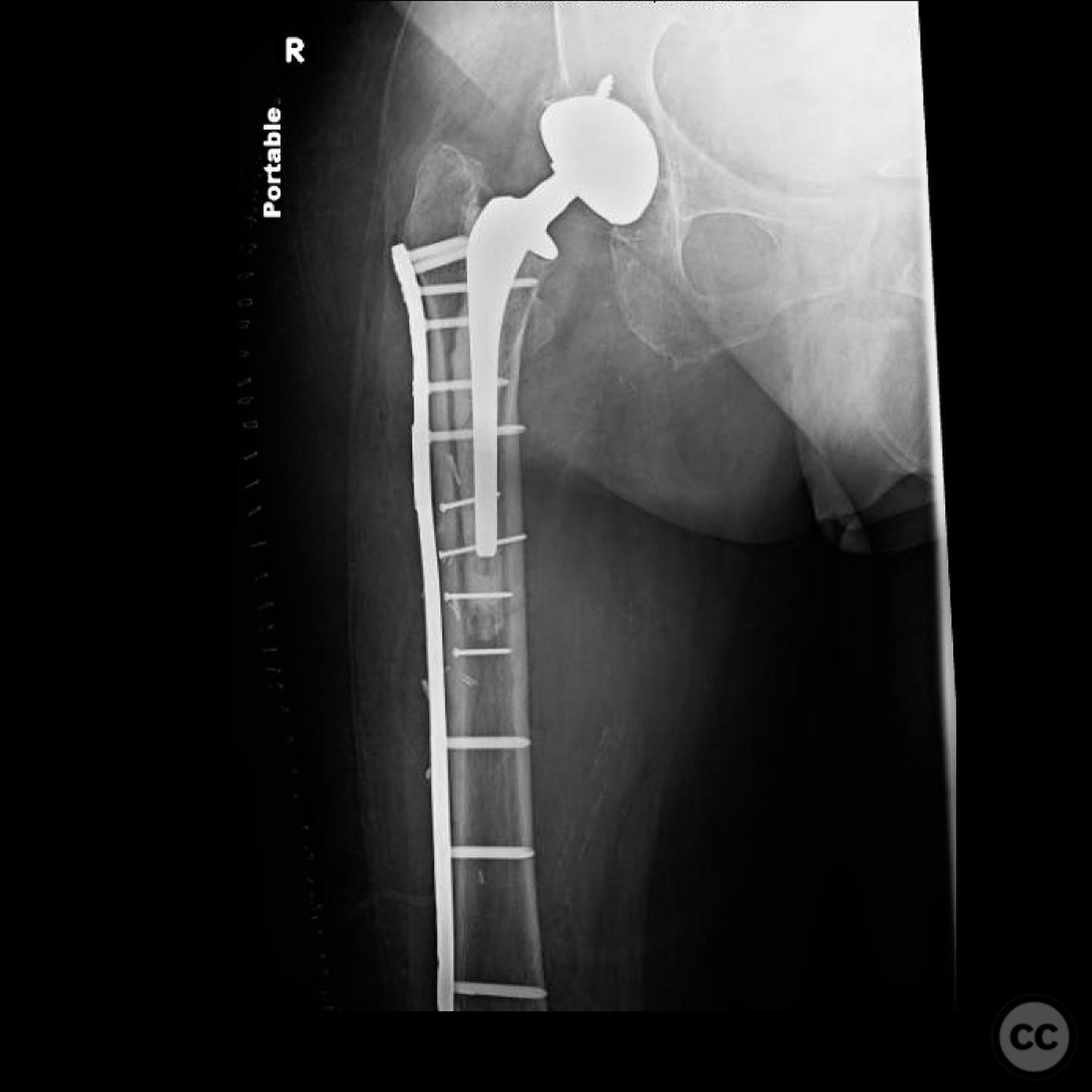
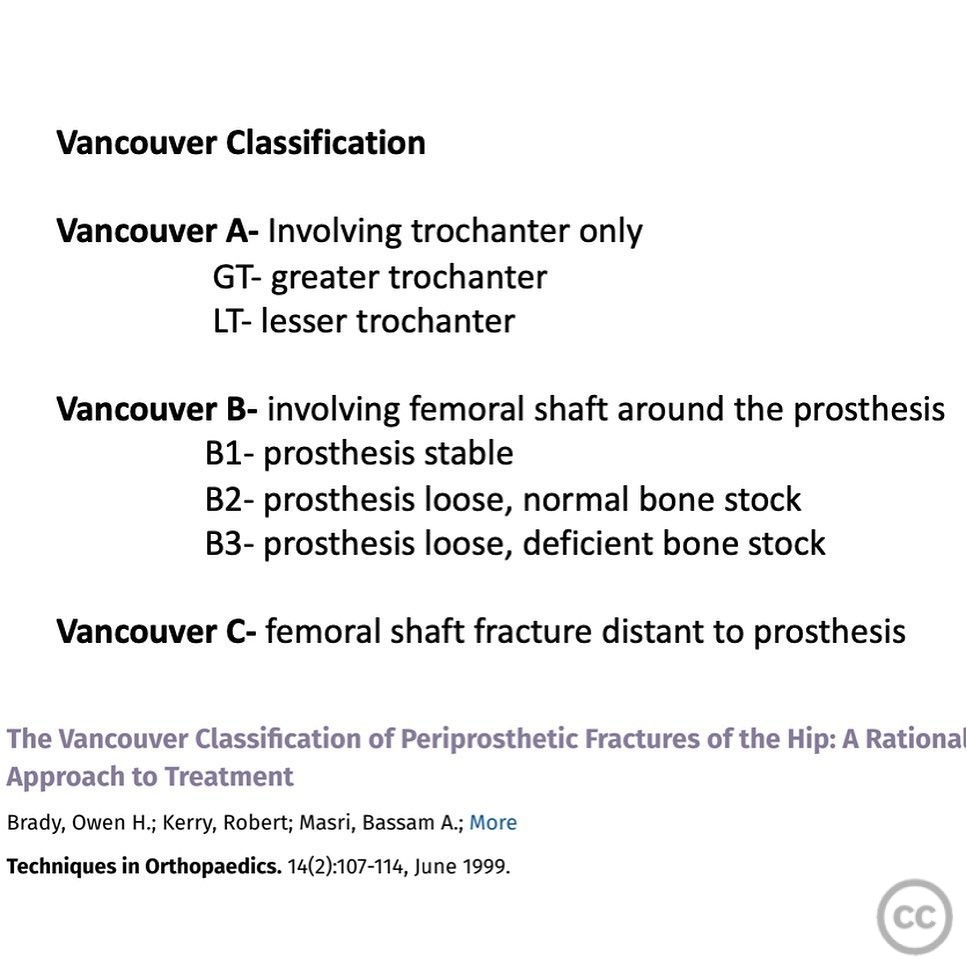
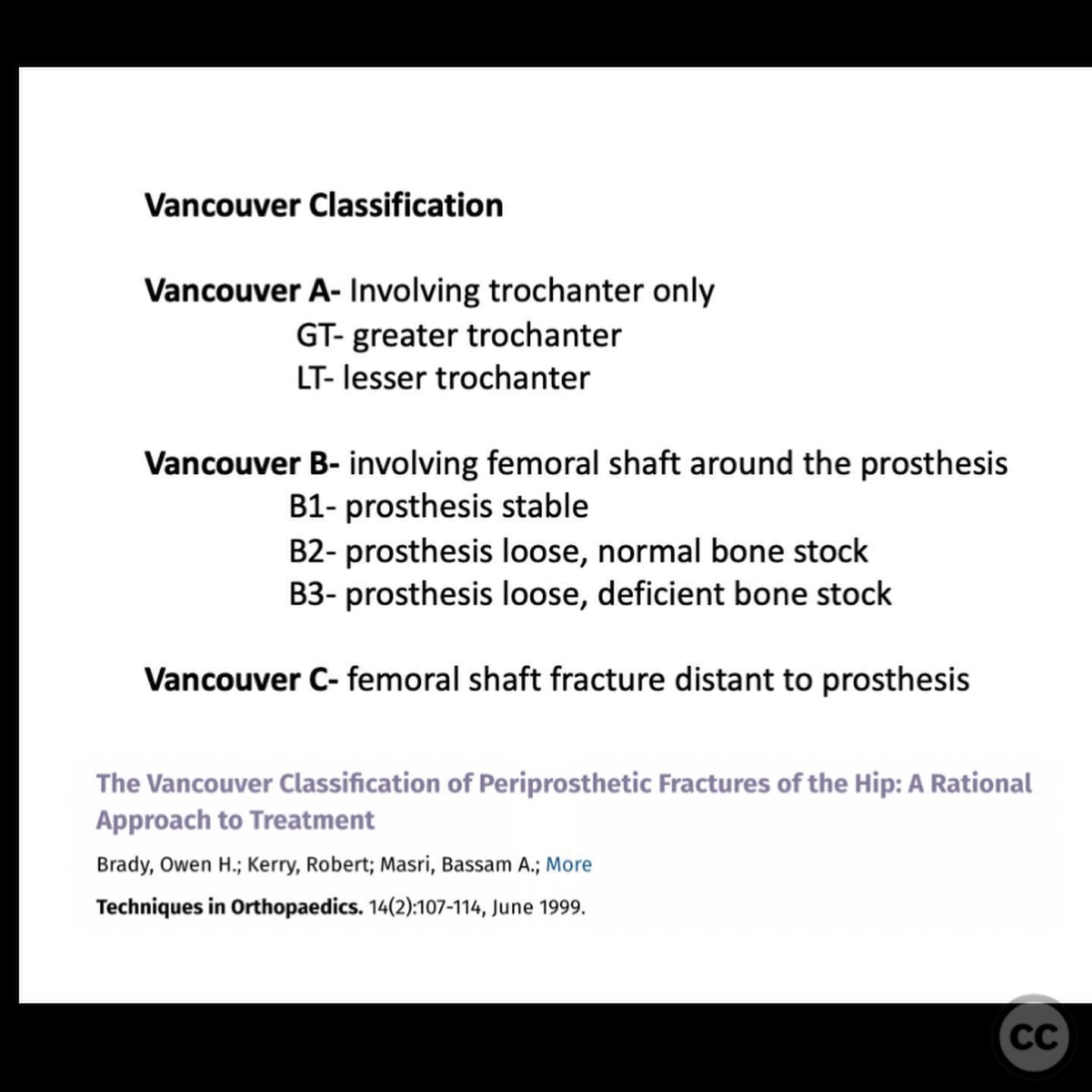
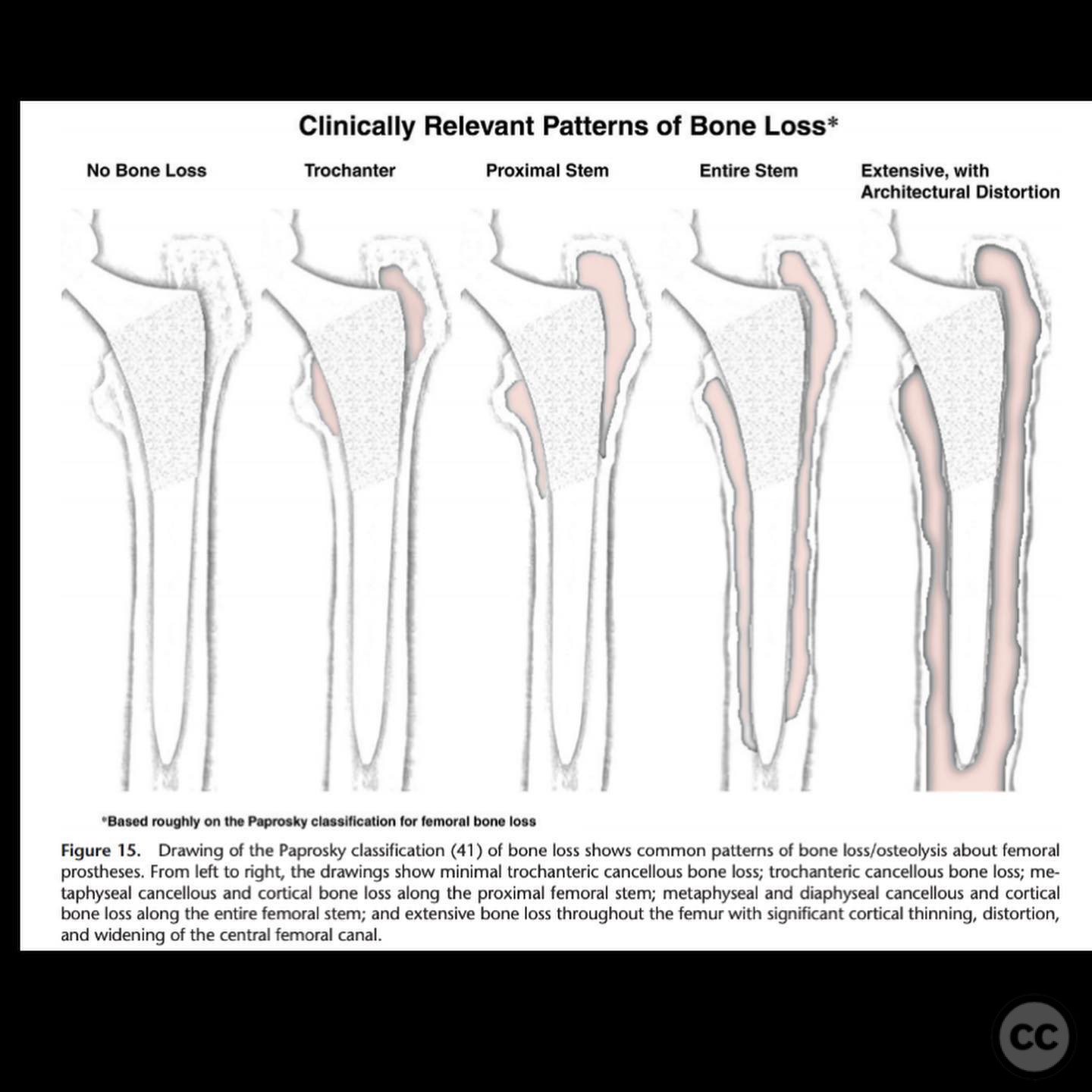
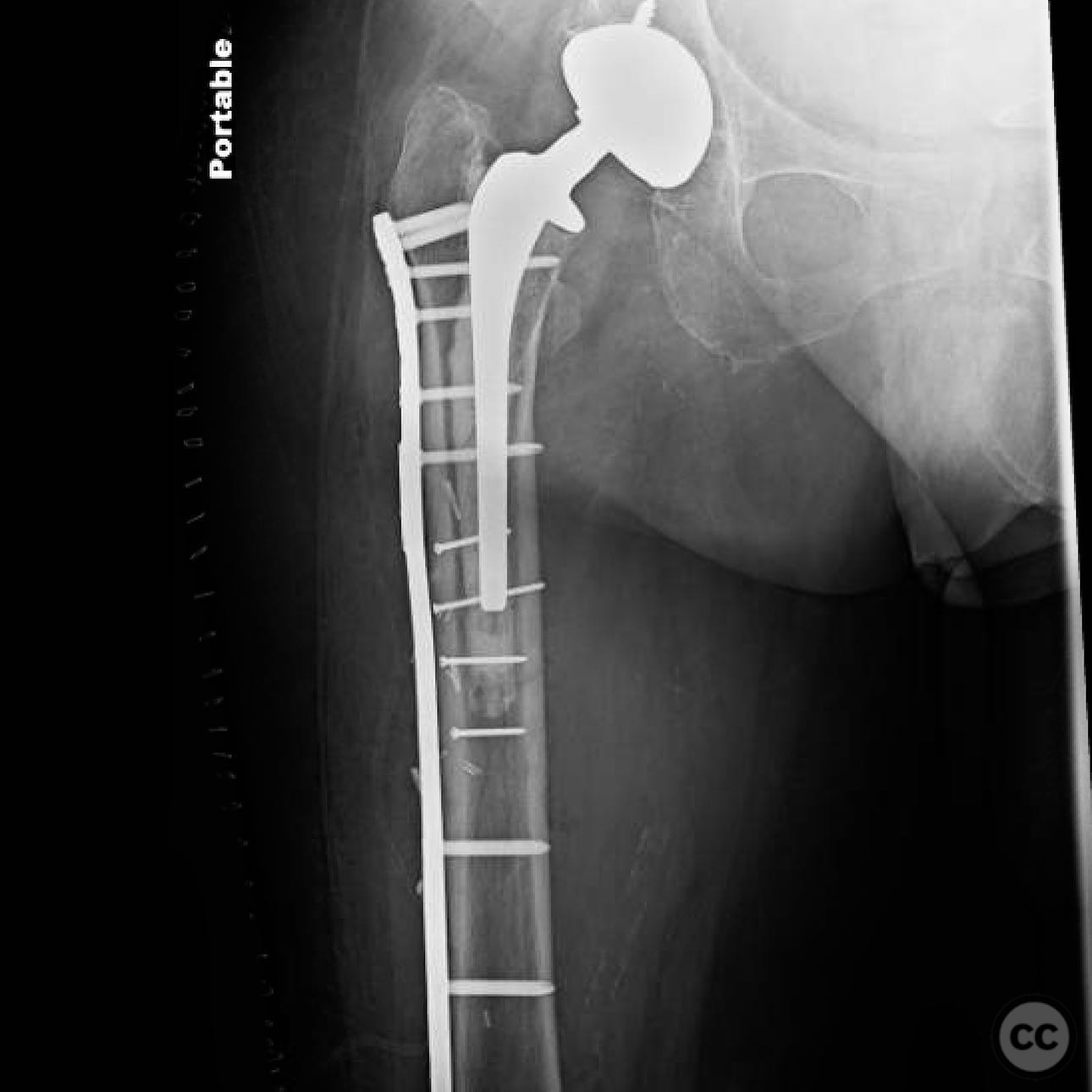
Clinical and radiological findings: An 88-year-old female, primarily a household ambulator, presented with a periprosthetic proximal femur fracture. The patient has a complex medical history including end-stage renal disease on hemodialysis, coronary artery disease, a pacemaker for complete heart block, and panhypopituitarism requiring steroid therapy. Radiological assessment confirmed a Vancouver B2 classification, indicating a fracture involving the prosthesis with a fractured cement mantle, suggesting a loose stem. Proximal femoral bone stock was deemed normal.
Preoperative Plan
Planning remarks: The preoperative plan involved an extensile lateral subvastus approach to directly expose the fracture site. The surgical strategy focused on achieving stable fixation with minimal operative time and blood loss, given the patient's limited physiological reserves.
Surgical Discussion
Patient positioning: The patient was positioned laterally to facilitate access to the proximal femur.
Anatomical surgical approach: An extensile lateral subvastus approach was utilized. Hemoclips were applied to all perforating vessels to minimize blood loss. Direct exposure of the fracture was achieved, followed by reduction and stabilization using clamps, lag screws, and a neutralization plate spanning the entire femur.
Operative remarks:The surgical team noted ongoing hemodynamic instability throughout the procedure, managed effectively by the anesthesia team. The decision to forego the typical revision to a long stem prosthesis was made in consideration of the patient's significant comorbidities and the need for rapid postoperative mobilization.
Postoperative protocol: The postoperative rehabilitation protocol allowed for weight-bearing as tolerated (WBAT) to facilitate early mobilization.
Follow up: Not specified.
Orthopaedic implants used: Neutralization plate, lag screws, hemoclips.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities






Article viewed 181 times
15 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Vancouver B2 Periprosthetic Femur Fracture in a High-Risk Patient. Journal of Orthopaedic Surgery and Traumatology. Case Report 45664161 Published Online Jul 15 2025.