Don’t Assume It’s a Simple Cyst: Biopsy First in Pediatric Pathologic Fractures
Score and Comment on this Case
Clinical Details
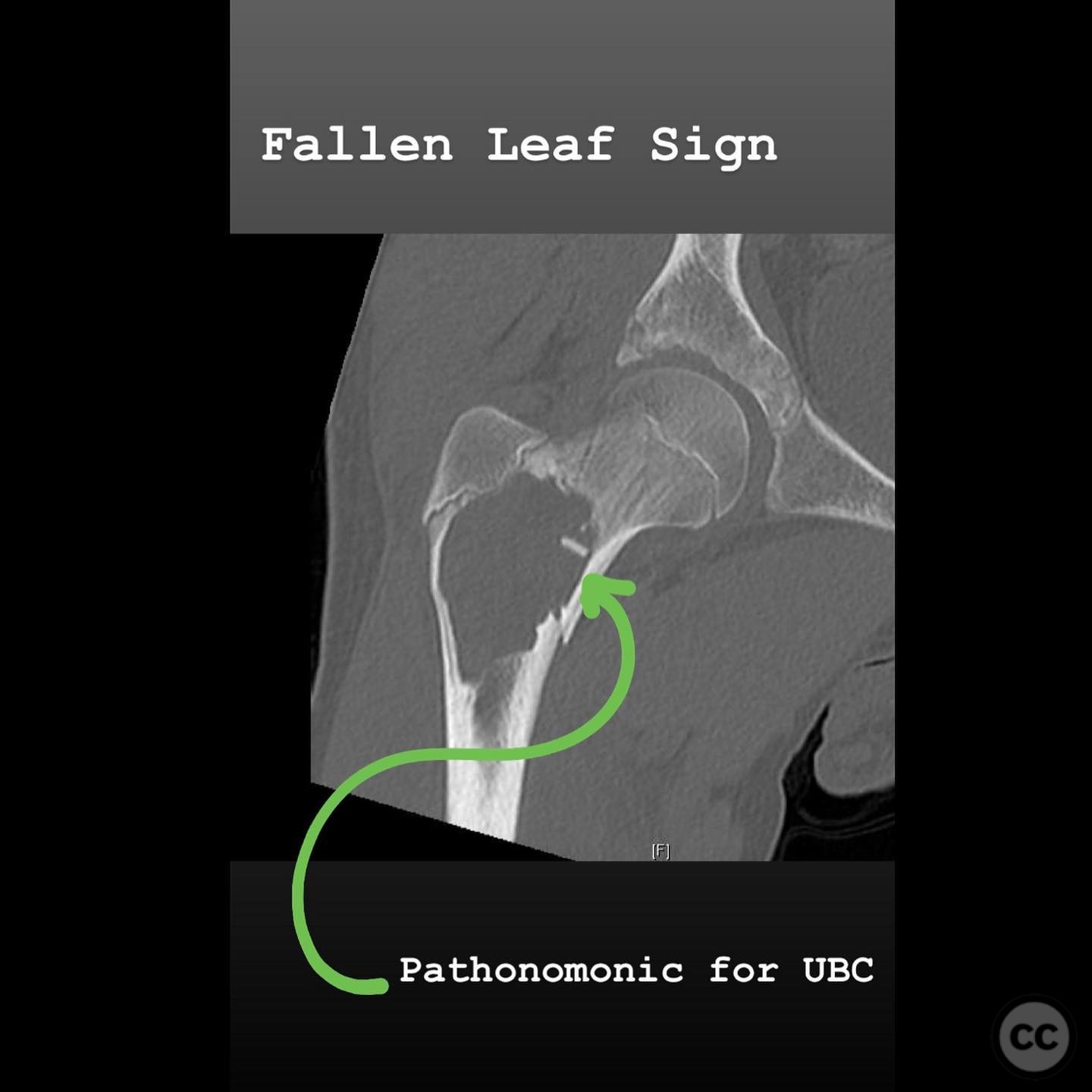
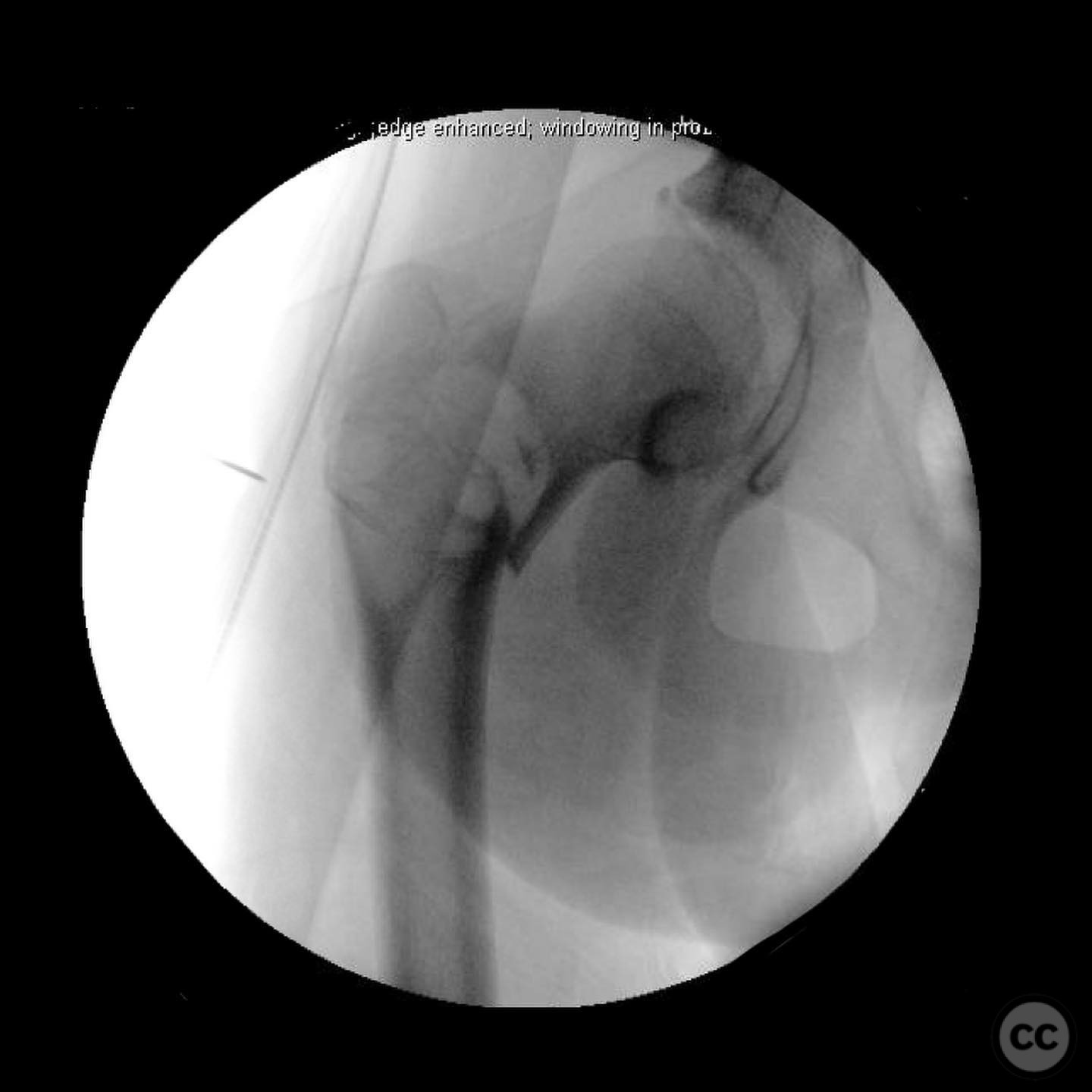
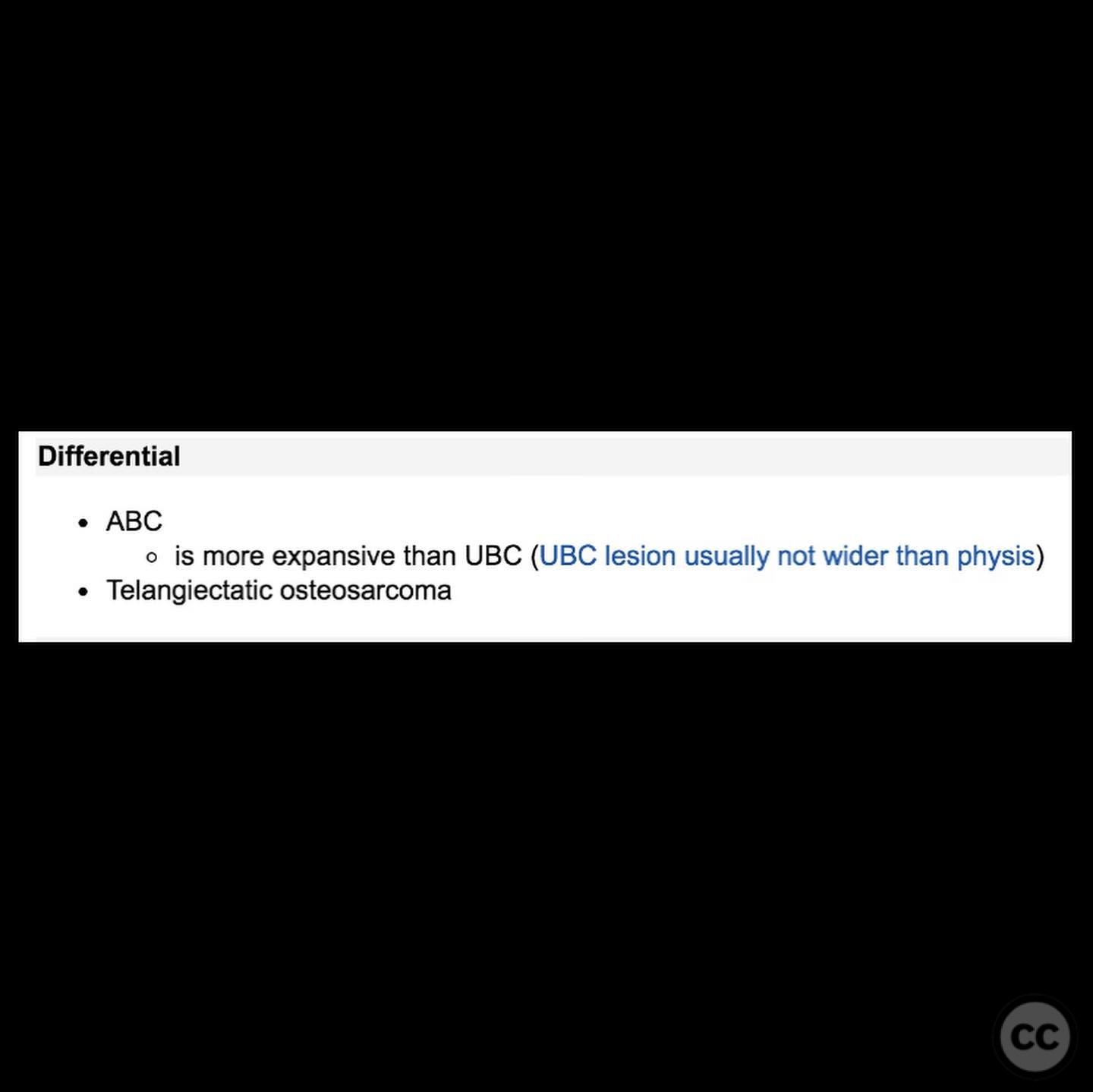
Clinical and radiological findings: A 14-year-old male presented with persistent groin pain after feeling a pop in the hip while wrestling. Radiological evaluation revealed a pathologic fracture of the proximal femur. Imaging demonstrated characteristics consistent with a unicameral bone cyst (UBC), including the classic "fallen leaf sign." Differential diagnosis included aneurysmal bone cyst (ABC) and telangiectatic osteosarcoma, necessitating further investigation.
Preoperative Plan
Planning remarks: The preoperative plan involved obtaining a biopsy of the lesion to rule out malignancy, specifically telangiectatic osteosarcoma, prior to surgical fixation. The surgical approach was planned to accommodate intramedullary nailing, given the proximal femur fracture configuration and the extent of the lesion.
Surgical Discussion
Patient positioning: The patient was positioned supine on a fracture table to facilitate intramedullary nailing of the proximal femur.
Anatomical surgical approach: A lateral approach to the proximal femur was utilized. The incision was made along the lateral aspect of the thigh, extending proximally to expose the entry point for intramedullary nailing. Careful dissection was performed to avoid damage to surrounding soft tissues.
Operative remarks:Intraoperative frozen section analysis confirmed no evidence of malignancy, allowing for continuation with surgical fixation. Prior to sending the specimen, the pathologist was informed:
> "I'm 98% certain this is a unicameral bone cyst, but I need you to rule out malignancy. Please confirm whether there is any nuclear atypia or overt malignancy. Also, ensure the specimen is adequate for final histological diagnosis. My differential includes telangiectatic osteosarcoma."
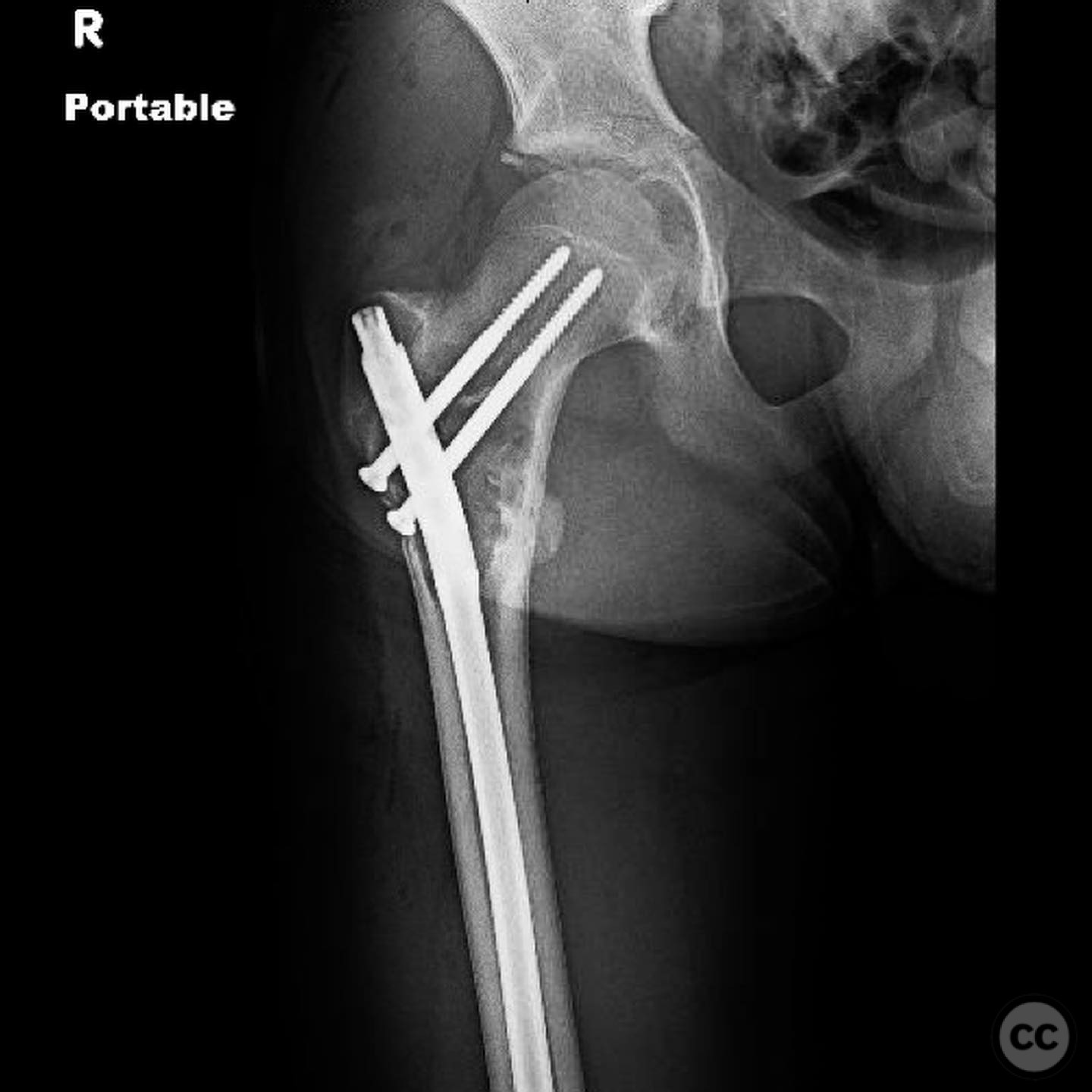
Due to significant thinning of the lateral wall and a fracture line extending proximal to where a sliding hip screw side plate would end, intramedullary nailing was chosen over a locking plate. Grafting was not performed in this case.
Postoperative protocol: Postoperative rehabilitation included non-weight bearing on the affected limb for 6 weeks, followed by gradual progression to full weight bearing as tolerated. Physical therapy focused on range of motion and strengthening exercises.
Follow up: Not specified.
Orthopaedic implants used: Intramedullary nail.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities





Article viewed 158 times
19 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Don’t Assume It’s a Simple Cyst: Biopsy First in Pediatric Pathologic Fractures. Journal of Orthopaedic Surgery and Traumatology. Case Report 45097058 Published Online Jul 19 2025.