Complex Tibial Reconstruction with Tibiotalar Arthrodesis Following Osteomyelitis and Bone Loss
Score and Comment on this Case
Clinical Details
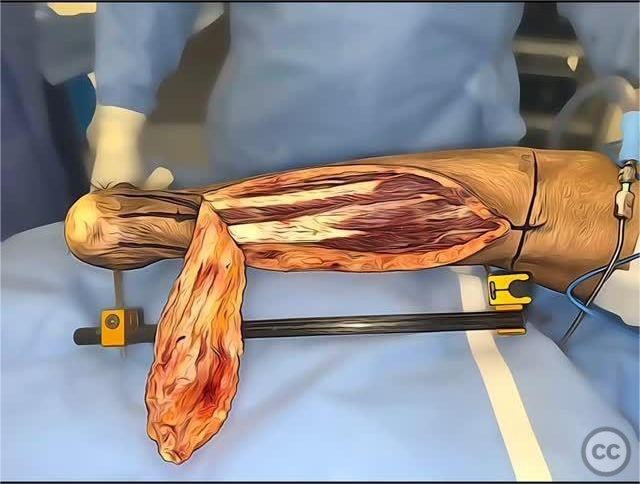
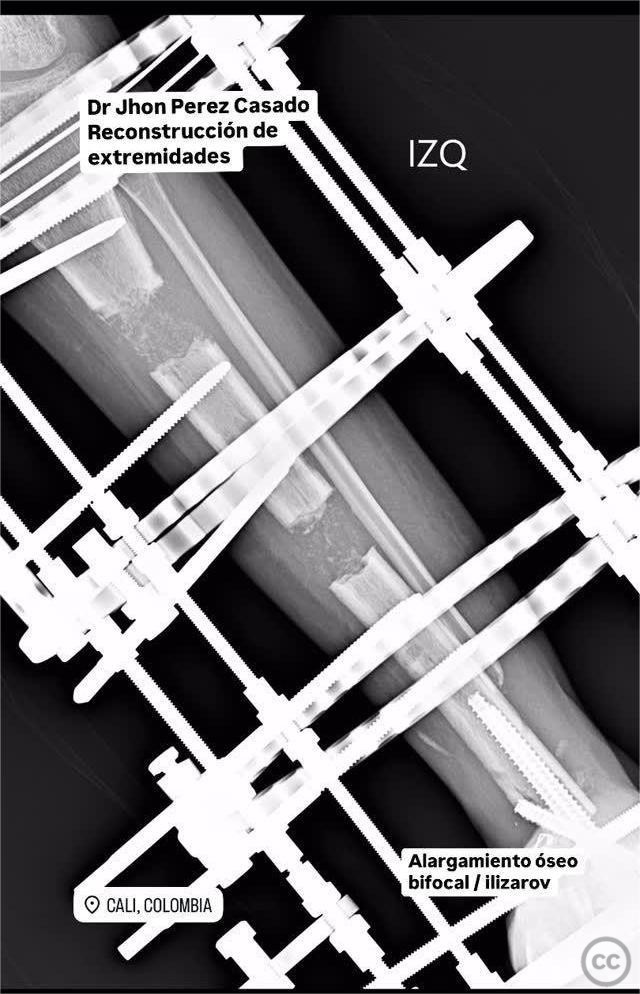
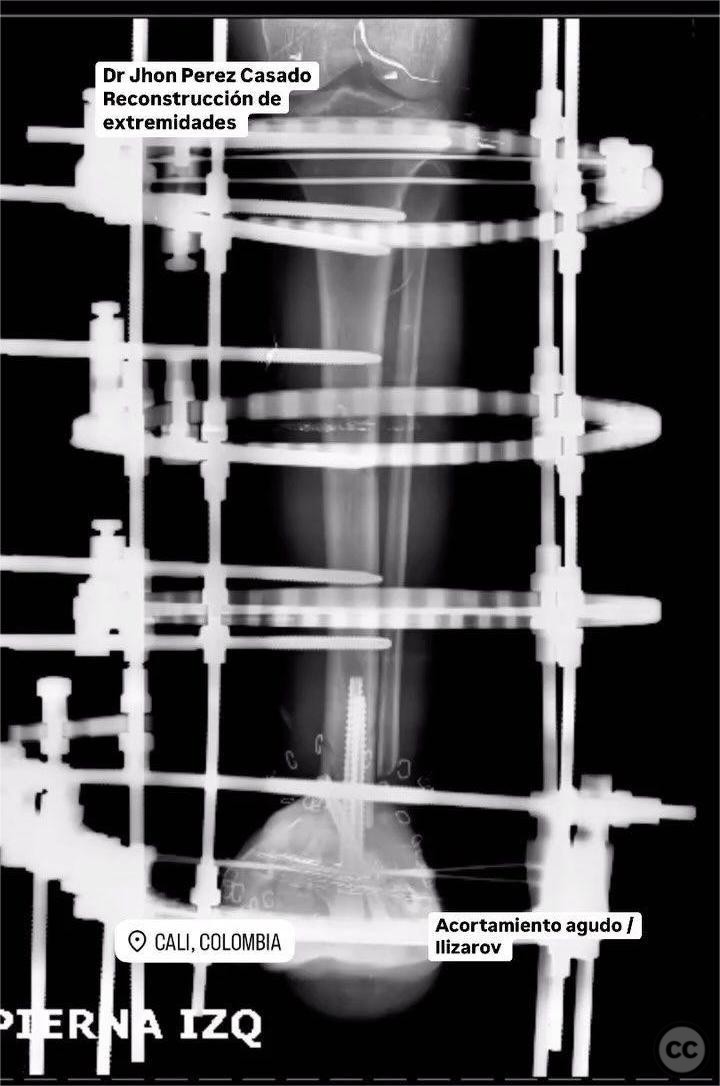
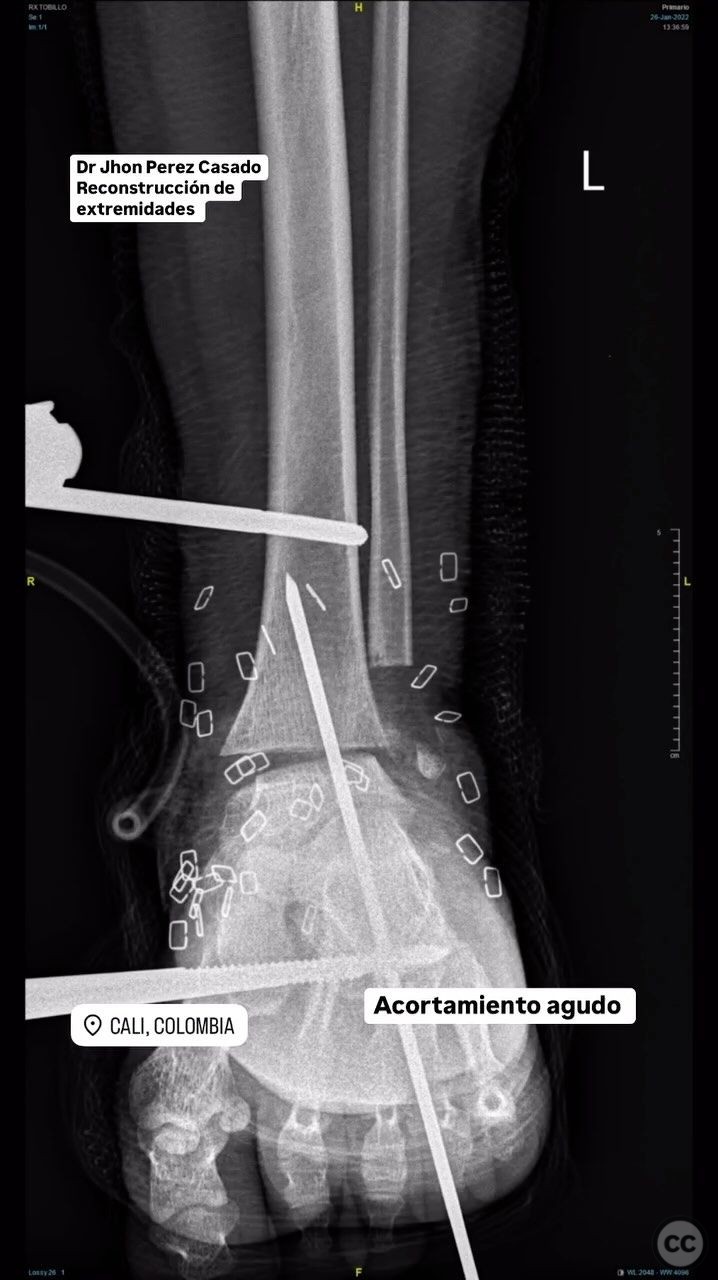
Clinical and radiological findings: The patient presented with an open fracture of the tibia accompanied by dislocation, complicated by osteomyelitis and significant bone loss. Initial management included surgical scrub and damage control for skin necrosis, followed by debridement and acute shortening. The fracture was initially stabilized using an Ilizarov external fixator, with subsequent bifocal bone lengthening. A sural perforator flap was utilized for soft tissue coverage. Radiological assessment indicated the need for staged bone reconstruction and eventual tibiotalar arthrodesis due to persistent ankle pain during ambulation.
Preoperative Plan
Planning remarks: The preoperative plan involved removal of the reverse tibial nail protector and obtaining cultures to assess infection status. Preparation for percutaneous tibiotalar arthrodesis was planned, utilizing ankle arthroscopy and application of bone morphogenetic protein (BMP) to enhance fusion.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table, with the affected limb elevated and supported to allow for optimal access to the tibial and ankle regions.
Anatomical surgical approach: A percutaneous approach was employed for the tibiotalar arthrodesis, facilitated by ankle arthroscopy. This minimally invasive technique allowed for direct visualization and preparation of the joint surfaces. Cannulated screws were inserted to achieve compression across the tibiotalar joint, with BMP applied to promote osseous integration and fusion.
Operative remarks:The surgeon noted that despite previous interventions, including transport lengthening and conversion to a nail, the patient continued to experience significant ankle pain upon walking. The decision to proceed with tibiotalar arthrodesis was made to address this issue. Intraoperatively, cultures were taken to ensure resolution of infection prior to definitive fusion. The use of BMP was intended to enhance the likelihood of successful arthrodesis.
Postoperative protocol: Postoperatively, the patient was advised to remain non-weight bearing on the affected limb for a period of 6 weeks, followed by gradual progression to partial weight bearing as tolerated. Physical therapy focused on maintaining range of motion in adjacent joints and strengthening exercises.
Follow up: Not specified.
Orthopaedic implants used: Ilizarov external fixator, reverse tibial nail, cannulated screws, bone morphogenetic protein (BMP).
Search for Related Literature

Jhon Perez Casado
- Colombia , Cali - Valle del Cauca
- Area of Specialty - Lower Limb
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities








Article viewed 171 times
21 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Perez Casado, J.J.. (2025). Complex Tibial Reconstruction with Tibiotalar Arthrodesis Following Osteomyelitis and Bone Loss. Journal of Orthopaedic Surgery and Traumatology. Case Report 44024261 Published Online Jul 21 2025.