Complex Right Femoral and Tibial Fracture Management with Early Total Care Approach
Score and Comment on this Case
Clinical Details
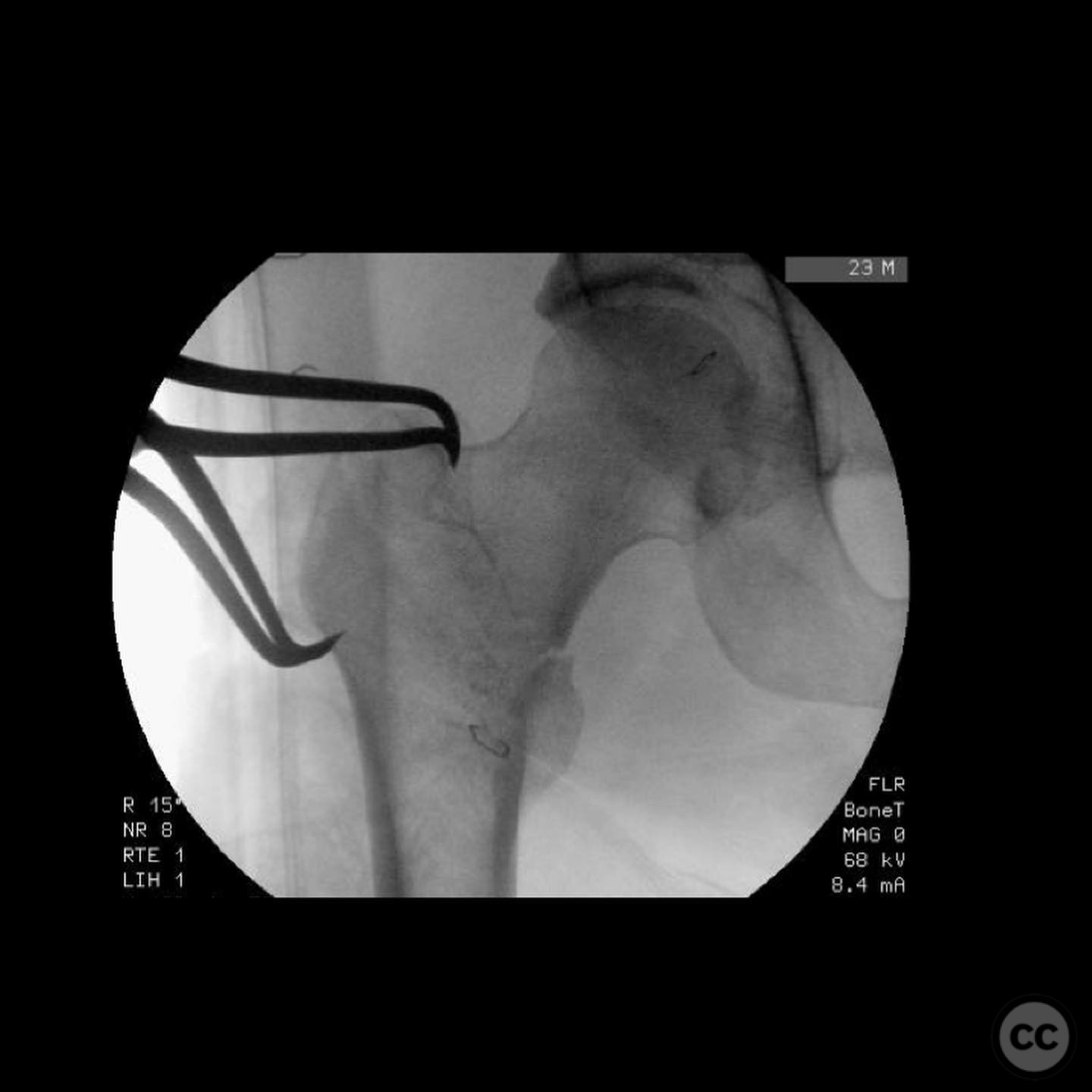
Clinical and radiological findings: A 44-year-old male involved in a motorcycle collision presented with a right-sided complex femoral and tibial fracture. The patient was hemodynamically stable with a lactate level of 1.5 mmol/L, indicating adequate resuscitation. No associated injuries to the abdomen, chest, head, or spine were noted. Radiological assessment revealed an intertrochanteric femoral fracture and a distal femoral split fracture, along with a tibial fracture with a critical size defect and proximal tibiofibular joint dislocation.
Preoperative Plan
Planning remarks: The preoperative plan involved a Watson-Jones approach for the intertrochanteric fracture, followed by stabilization using an anti-rotation screw and a sliding hip screw side plate. The distal femoral split fracture was to be clamped and fixed prior to retrograde nailing. Standard tibial nailing was planned with the Masquelet technique for the critical size defect.
Surgical Discussion
Patient positioning: The patient was positioned supine on a flat-top operating table with a small bump placed under the hip to facilitate access to the surgical sites.
Anatomical surgical approach: A Watson-Jones approach was utilized for the intertrochanteric fracture, involving an incision over the lateral aspect of the hip, with dissection through the interval between the tensor fasciae latae and gluteus medius muscles to expose the proximal femur. For the distal femur, a lateral approach was employed to allow for clamping and fixation of the split fracture. Standard anterior approach for tibial nailing was used, with attention to the proximal tibiofibular joint dislocation.
Operative remarks:The surgical procedure began with open clamping of the intertrochanteric fracture, followed by fixation using an anti-rotation screw and sliding hip screw side plate, initially securing only the top screw in the side plate. The distal femur split was clamped and fixed, allowing for retrograde nailing. During tibial nailing, a Masquelet technique was employed for the critical size defect, utilizing antibiotic-loaded cement spacer. The proximal tibiofibular joint dislocation was noted intraoperatively.
Postoperative protocol: Postoperatively, partial weight-bearing was initiated at 7 weeks, progressing to full weight-bearing by 3 months post-index operation. At 5 weeks, the patient underwent removal of the cement spacer and bone grafting using RIA autograft expanded with allograft.
Follow up: At 2 years follow-up, the patient demonstrated solid bone healing. At 9 months postoperatively, consolidation was achieved, and at 1.5 years, removal of the distal femoral blade plate and bothersome bolts was performed.
Orthopaedic implants used: Anti-rotation screw, sliding hip screw side plate, retrograde femoral nail, tibial nail, Masquelet cement spacer with antibiotics.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities

















Article viewed 144 times
21 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Complex Right Femoral and Tibial Fracture Management with Early Total Care Approach. Journal of Orthopaedic Surgery and Traumatology. Case Report 42785046 Published Online Jul 21 2025.