Expeditious Reduction of Bleeding Both Column Acetabular Fracture
Score and Comment on this Case
Clinical Details
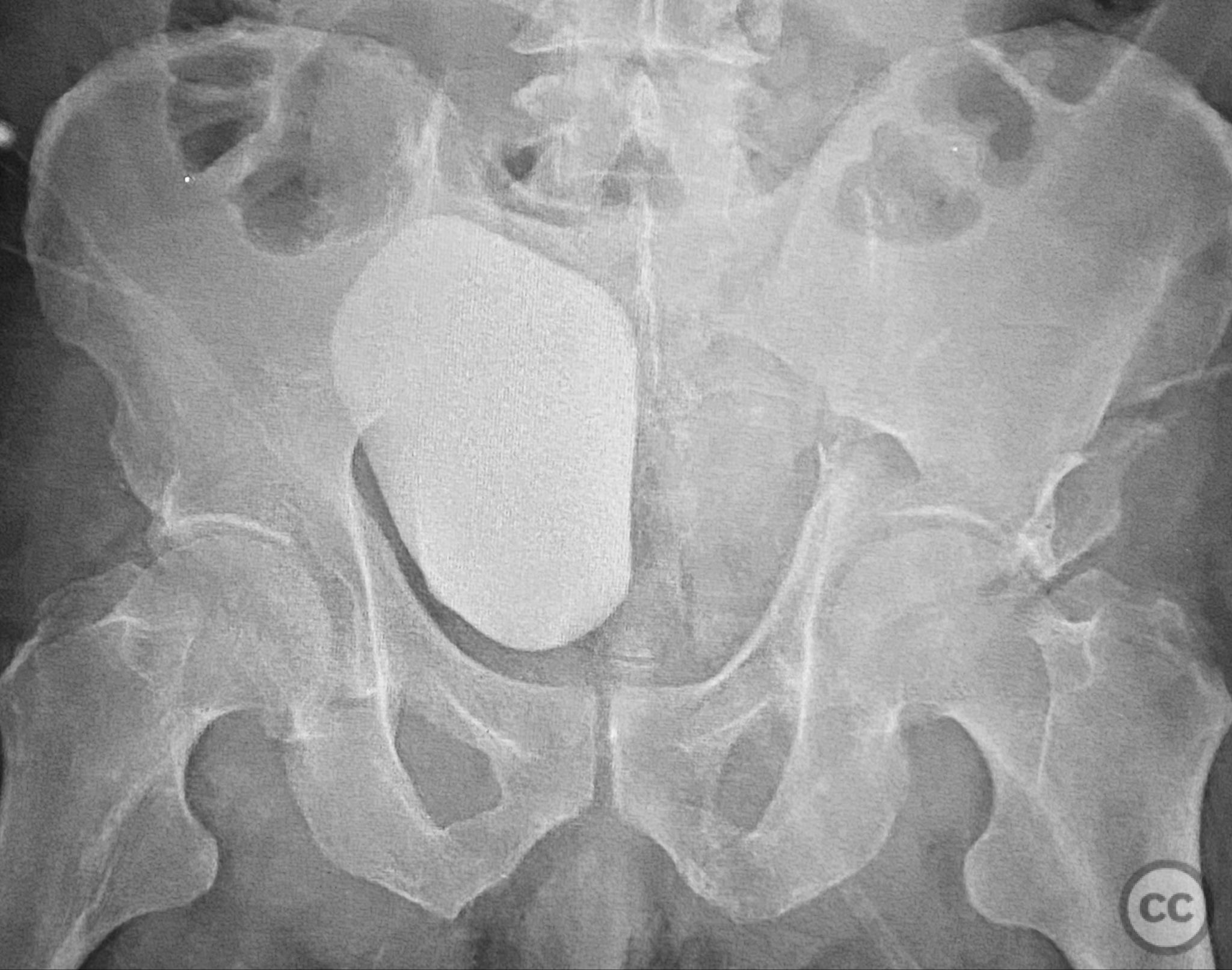
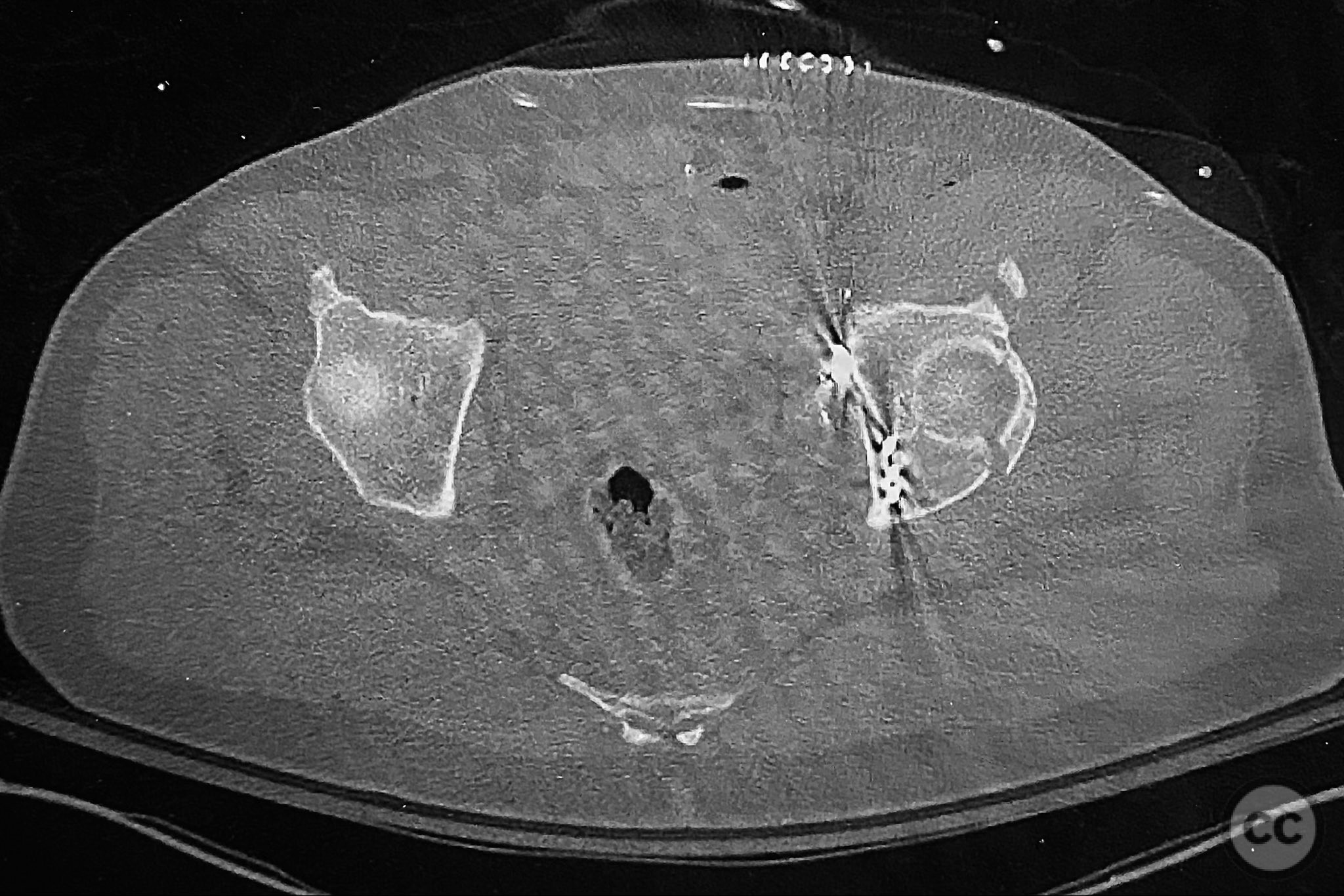
Clinical and radiological findings: A patient presented with a left-sided both column acetabular fracture, classified as AO/OTA 62C, following trauma. Initial plain pelvic radiographs and axial computed tomography demonstrated displacement of the urinary bladder, most likely secondary to acute hemorrhage from the fracture surfaces. No further details regarding associated injuries or neurovascular status were provided.
Preoperative Plan
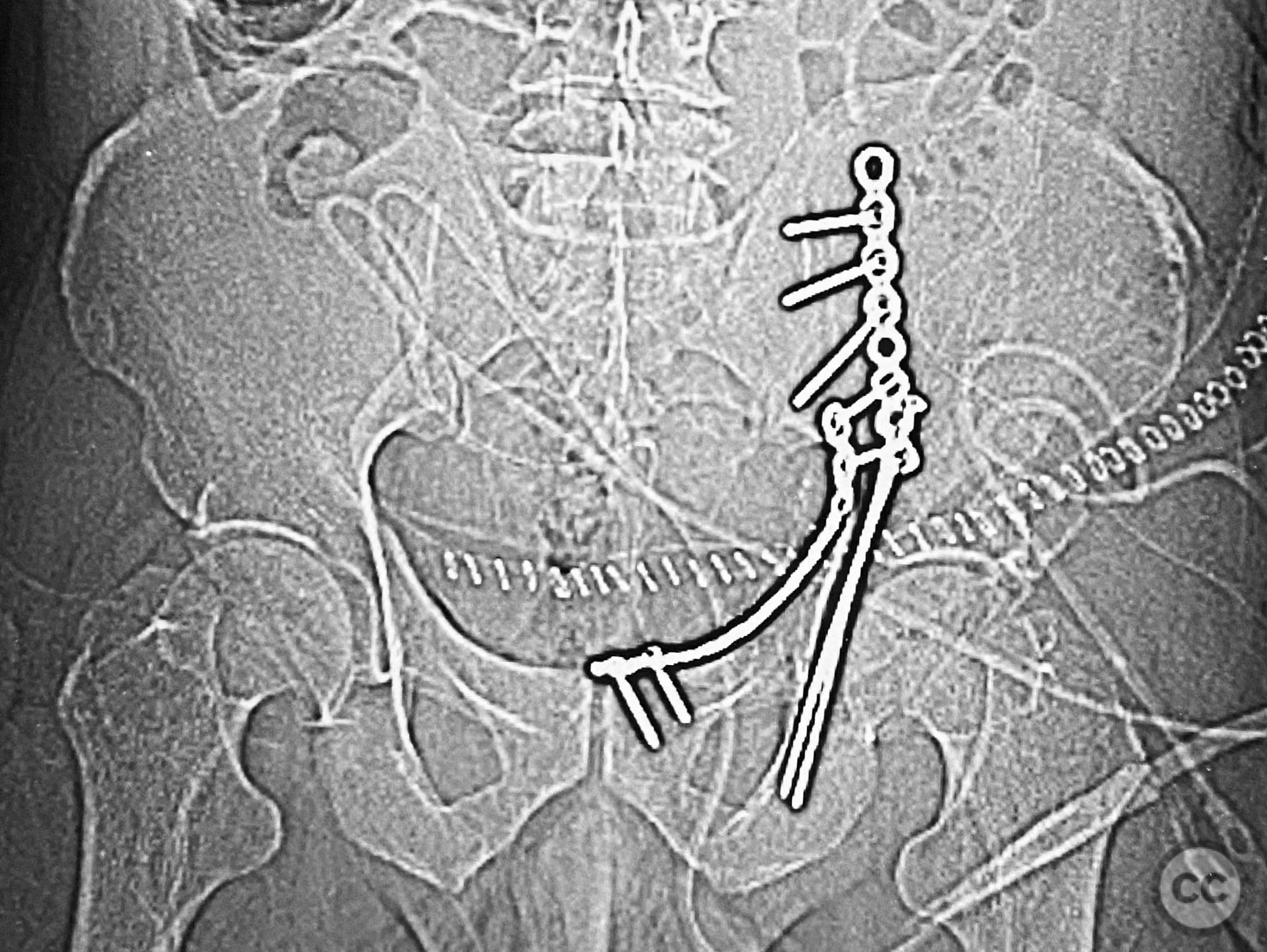
Planning remarks: The preoperative technical plan included preparation for urgent control of intraoperative hemorrhage from the acetabular fracture surfaces. The surgical approach was planned as an ilioinguinal exposure to facilitate rapid access to both columns of the acetabulum, with readiness for immediate reduction and hemostasis.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent operating table to allow for anterior pelvic access and intraoperative fluoroscopic imaging.
Operative remarks:Upon exposure, the acetabular fracture surfaces exhibited brisk arterial bleeding. The fracture site was rapidly irrigated and cleared of hematoma. Manual longitudinal traction was applied to the limb, and a spiked pusher was used to achieve prompt reduction of the anterior column fragment. This maneuver resulted in immediate cessation of fracture-related hemorrhage. The case highlights the necessity for preoperative planning that anticipates significant intraoperative bleeding in both column acetabular fractures, and emphasizes the importance of expeditious reduction as a hemostatic measure.
Postoperative protocol: Postoperatively, the patient was maintained non-weight bearing on the affected limb for six weeks, with early initiation of passive range of motion exercises as tolerated.
Follow up: Not specified
Orthopaedic implants used: Spiked pusher (reduction instrument)
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities


Article viewed 189 times
02 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Expeditious Reduction of Bleeding Both Column Acetabular Fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 42537736 Published Online Sep 02 2025.