Complex Both-Column Acetabular Fracture in Obese Senior with Prior Abdominal Surgery and Lap Belt Injury
Score and Comment on this Case
Clinical Details
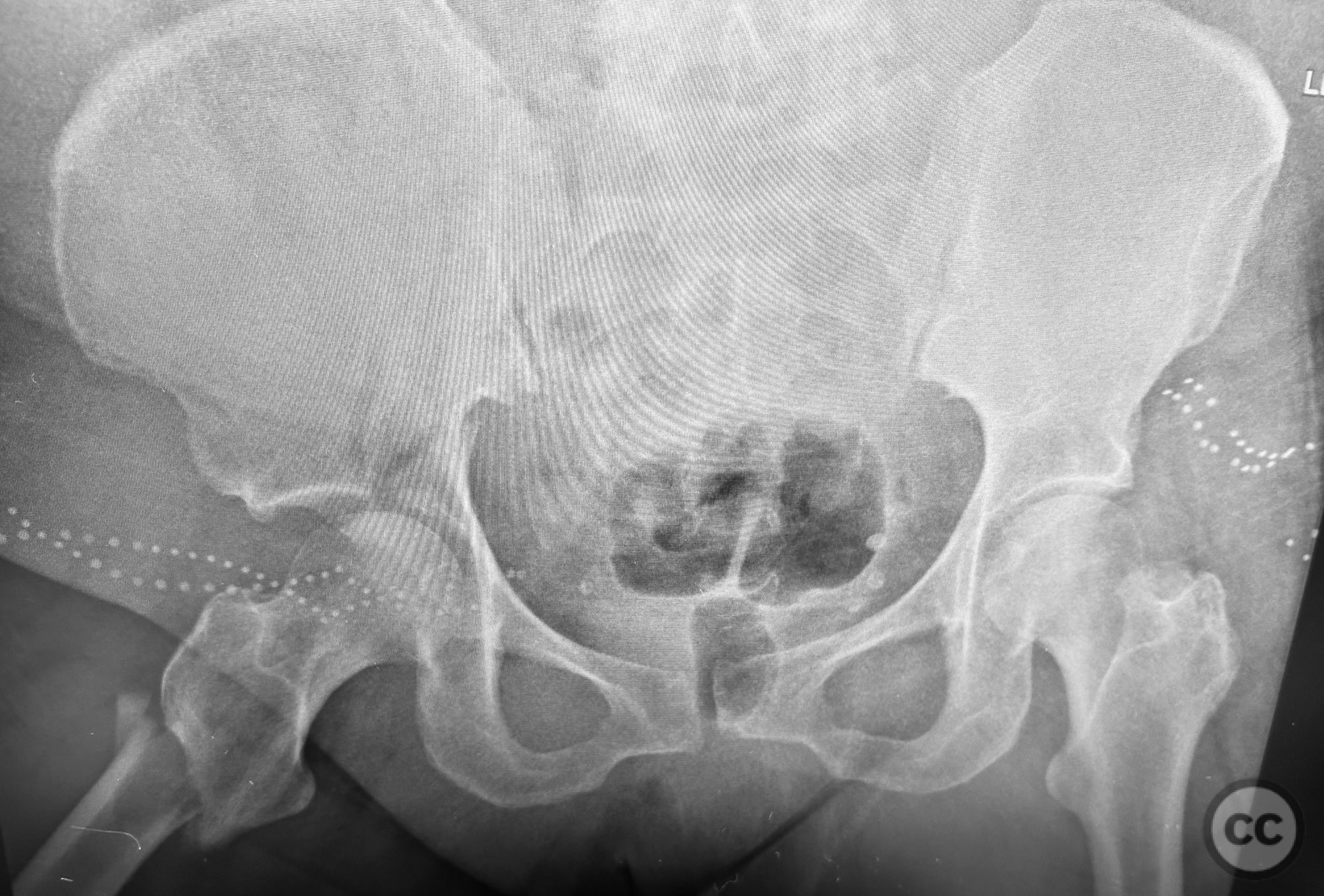
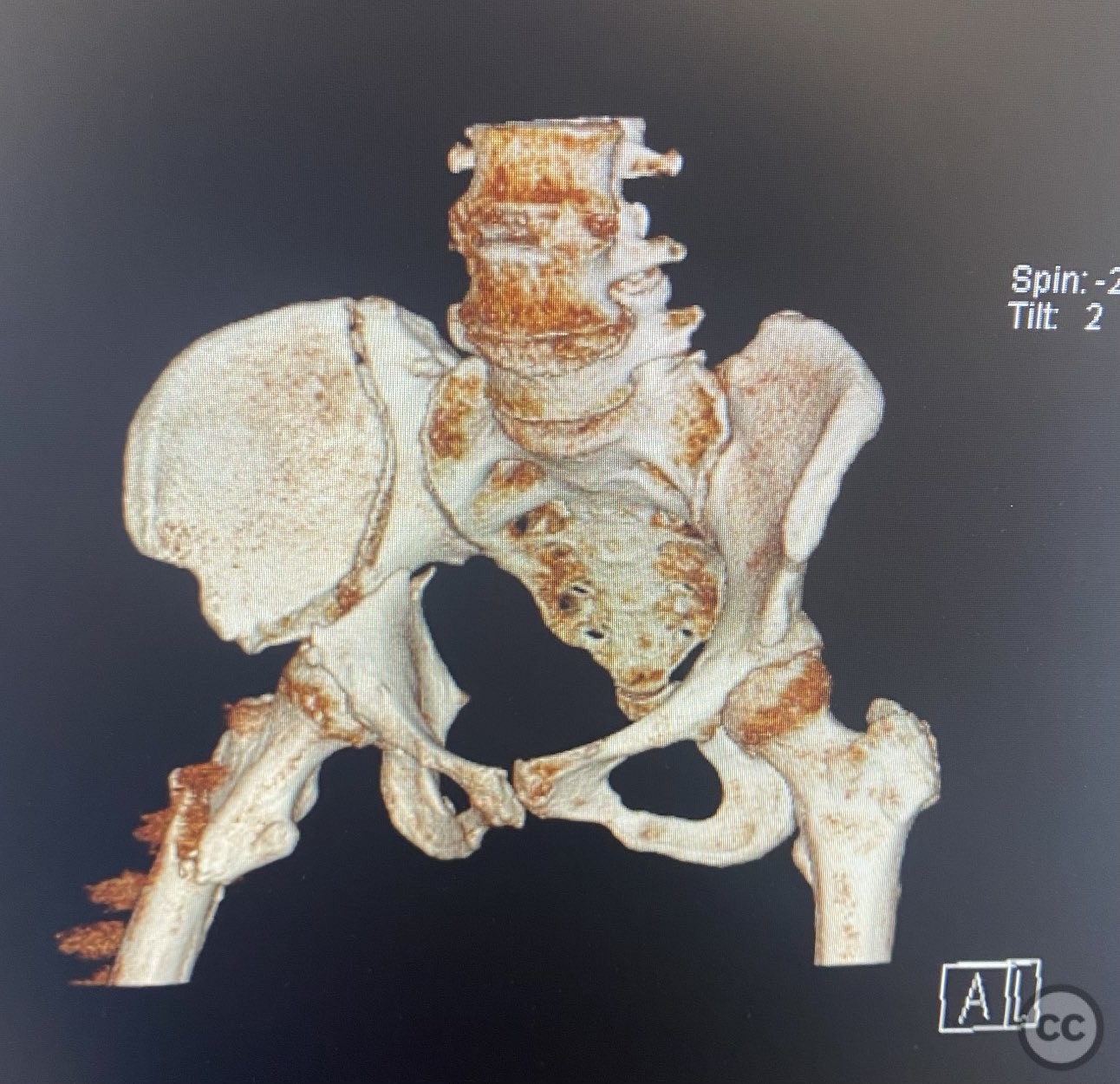
Clinical and radiological findings: An active but obese senior patient presented with a complex acetabular fracture following a lap belt injury. The patient had significant anterior abdominal surgical scarring from prior gynecological operations. Initial clinical assessment revealed a closed injury with associated soft tissue trauma in the inguinal and lower abdominal regions. Radiographs and computed tomography demonstrated an AO/OTA 62C1 (AsBothCol) pattern, with both anterior and posterior column involvement and displacement. There was no evidence of neurovascular compromise. Notably, the lap belt injury zone showed extensive soft tissue contusion and devitalization.
Preoperative Plan
Planning remarks: The preoperative plan was for open reduction and internal fixation via an ilioinguinal approach, utilizing the lateral and middle windows to access the anterior column, pelvic brim, and quadrilateral surface. The plan included direct visualization and debridement of devitalized tissues, anatomic reduction of fracture surfaces using clamp-assisted techniques, and definitive fixation with lag screws and a neutralization plate. Inguinal zone traumatic injuries were to be repaired concurrently.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent table, with a bump under the ipsilateral flank to facilitate exposure of the hemipelvis. The ipsilateral lower limb was draped free to allow manipulation during reduction.
Anatomical surgical approach: A standard ilioinguinal approach was performed, utilizing the lateral and middle intervals. The incision was made parallel to the inguinal ligament, extending from the anterior superior iliac spine (ASIS) towards the pubic tubercle. Subcutaneous tissues were dissected to expose the external oblique aponeurosis, which was incised in line with its fibers. The lateral window was developed by retracting the iliacus muscle from the internal iliac fossa, while the middle window was created by mobilizing the external iliac vessels medially. Careful subperiosteal dissection exposed the pelvic brim, quadrilateral plate, and both columns. The lap belt injury zone was debrided of necrotic tissue, and traumatic defects in the inguinal region were repaired.
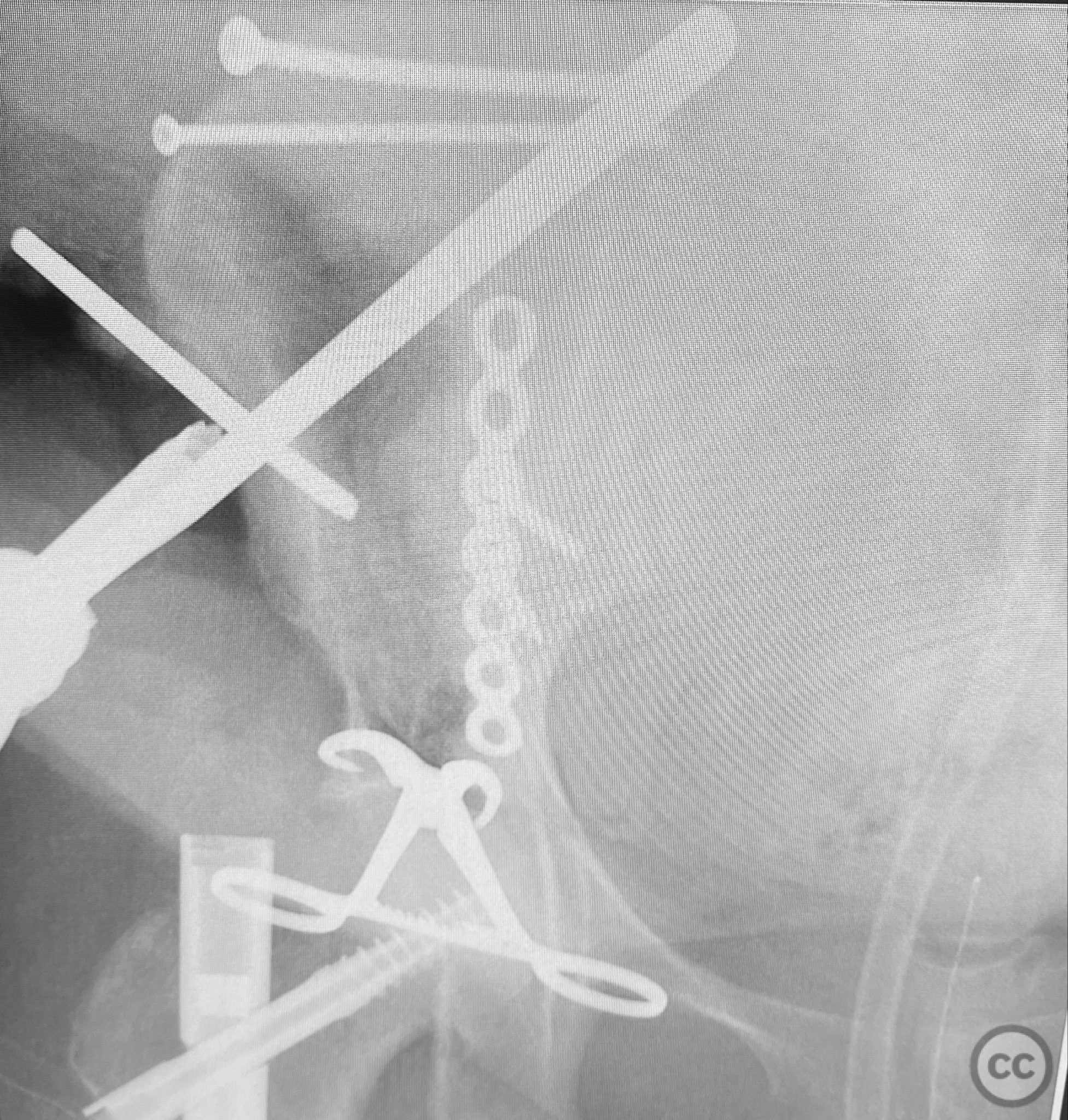
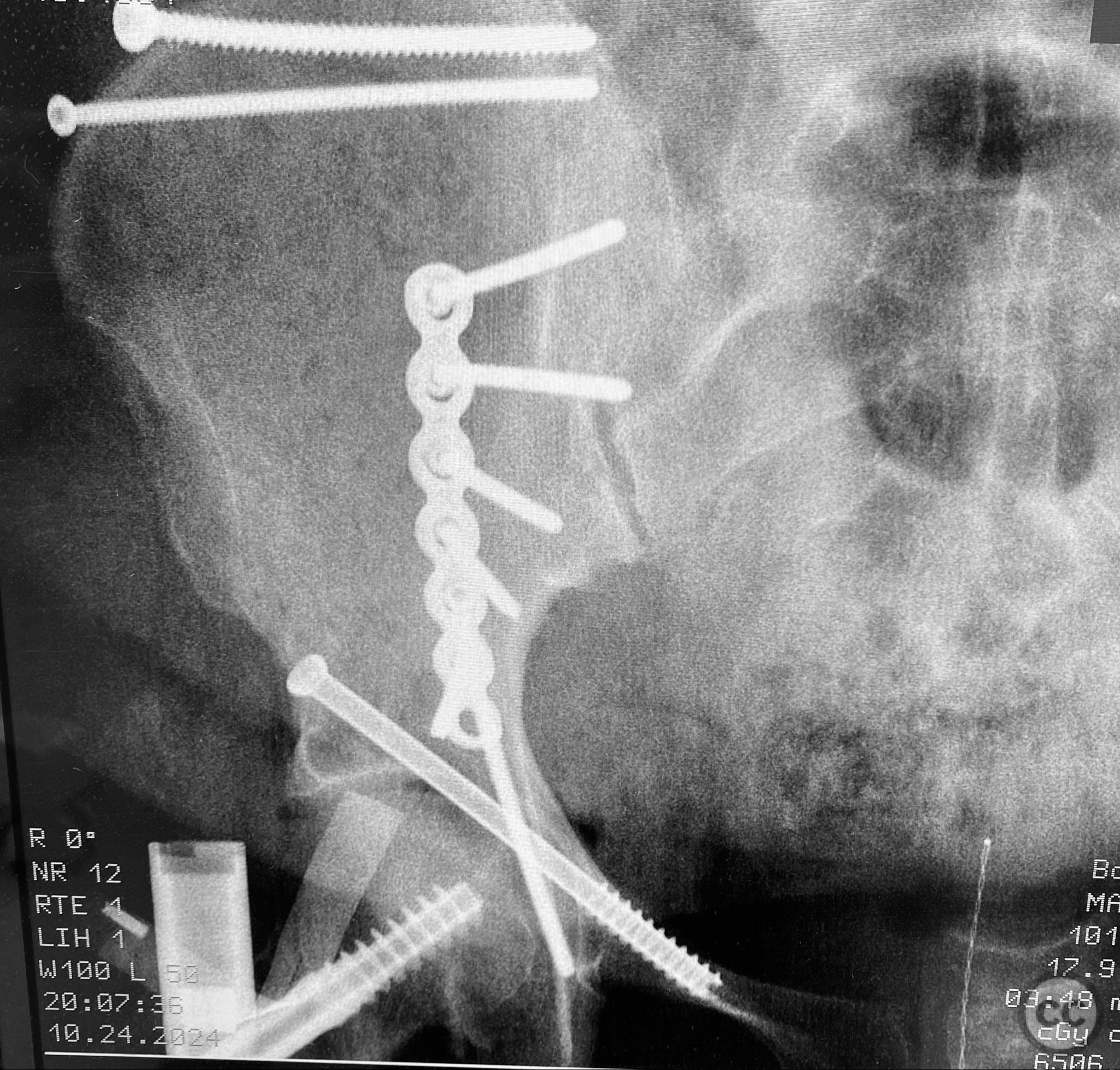
Operative remarks:Due to significant obesity and depth of exposure, visualization of fracture surfaces required meticulous retraction and soft tissue management. Reduction was achieved using a combination of colinear clamps (applied via an iliac manipulative pin) and medium tenaculum clamps (secured through a medial bone hole). These clamps maintained reduction without obstructing subsequent implant placement. The sequence of fixation was: first, lag screws were placed across the iliac crest fracture components; second, a neutralization plate was applied along the pelvic brim with additional lag screws securing the anterior column; third, a percutaneous cannulated lag screw was inserted across the superior pubic ramus. A brim medullary screw was deliberately avoided to prevent obstruction of optimal implant placement. The plate functioned primarily as a linear washer for the lag screws rather than as a load-bearing device.
Postoperative protocol: Postoperatively, the patient was maintained non-weight bearing on the affected limb for six weeks, with immediate initiation of passive range-of-motion exercises for hip and knee. Progressive weight bearing was introduced at eight weeks postoperatively, contingent on radiographic evidence of healing.
Follow up: Not specified
Orthopaedic implants used: 3.5mm pelvic reconstruction plate; multiple 3.5mm cortical lag screws; 6.5mm cannulated lag screw
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities

Article viewed 107 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Complex Both-Column Acetabular Fracture in Obese Senior with Prior Abdominal Surgery and Lap Belt Injury. Journal of Orthopaedic Surgery and Traumatology. Case Report 41517433 Published Online Sep 11 2025.