From Failure to Function: Staged Correction of Varus-Procurvatum Malunion and Medial Femoral Condyle Fracture in a Steroid-Dependent Patient"
Score and Comment on this Case
Clinical Details
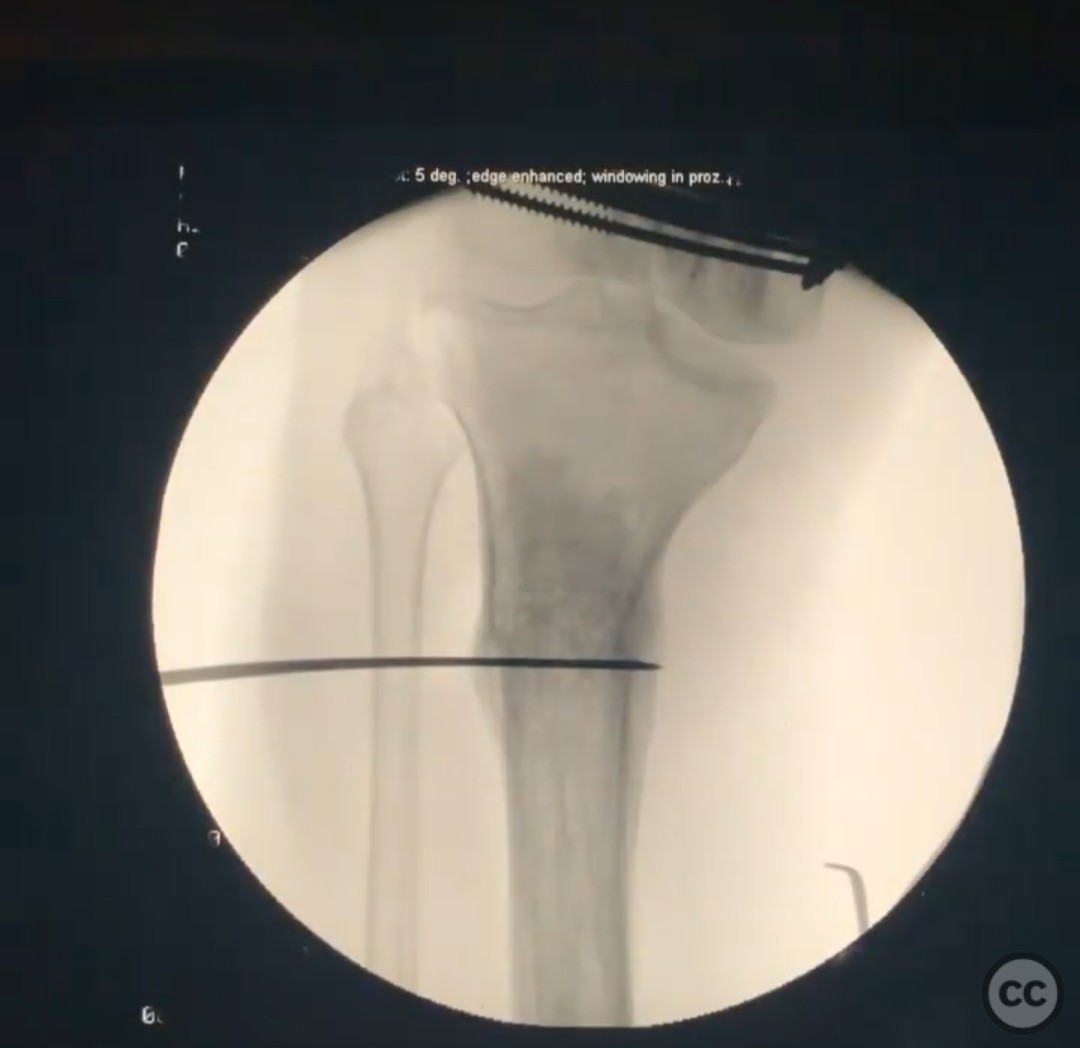
Clinical and radiological findings: A 57-year-old female with a history of a rare autoimmune condition treated with chronic high-dose oral steroids presented with a medial femoral condyle fracture, proximal tibial malunion, and a healed ankle arthrodesis. The patient had previously sustained a trimalleolar fracture dislocation, which was initially managed non-operatively and subsequently required a hindfoot fusion nail due to failure of conservative treatment. She later sustained a proximal tibial fracture that healed in varus and procurvatum following non-operative management. The patient reported difficulty ambulating and experienced another fall, resulting in the medial femoral condyle fracture. Radiological assessment confirmed the presence of the medial femoral condyle fracture and malunited proximal tibia.
Preoperative Plan
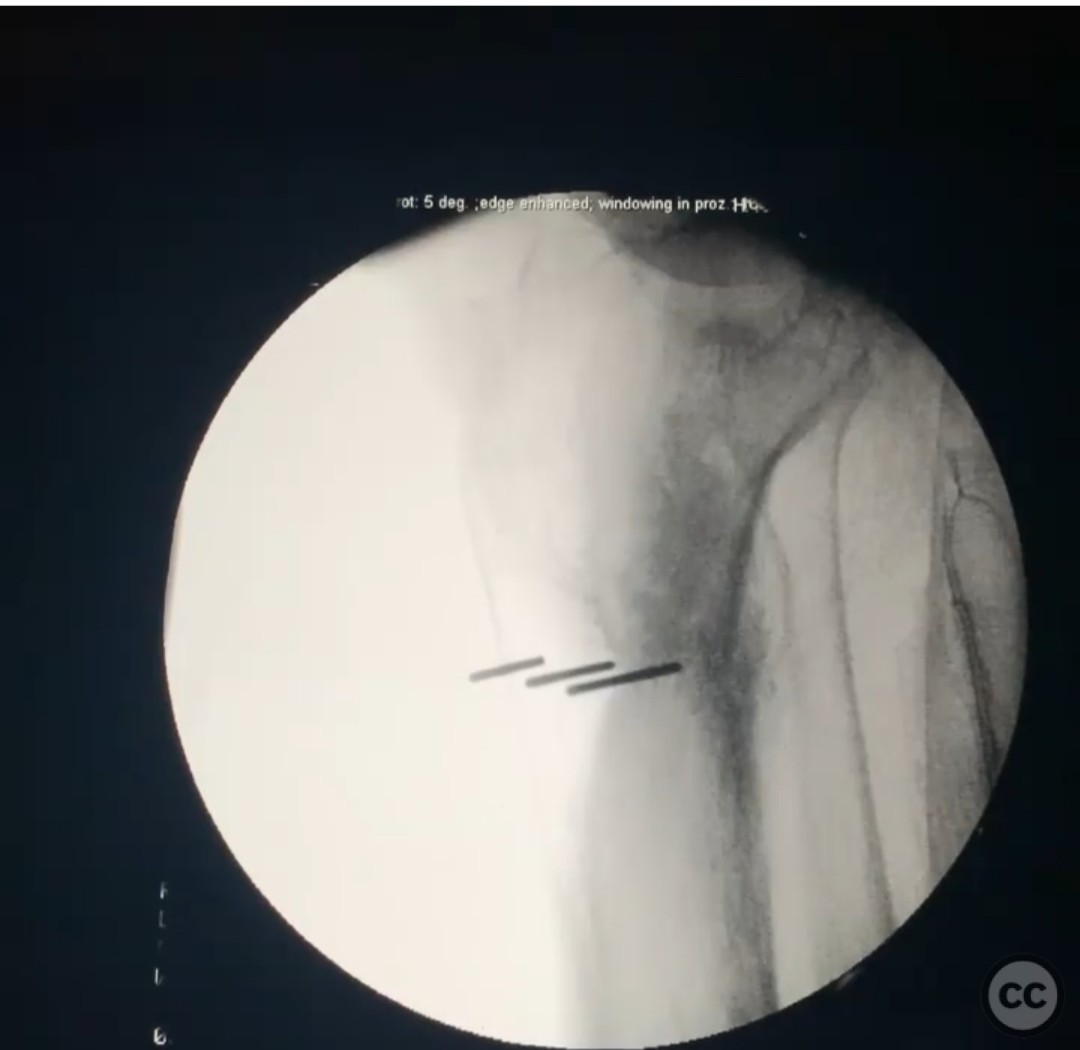
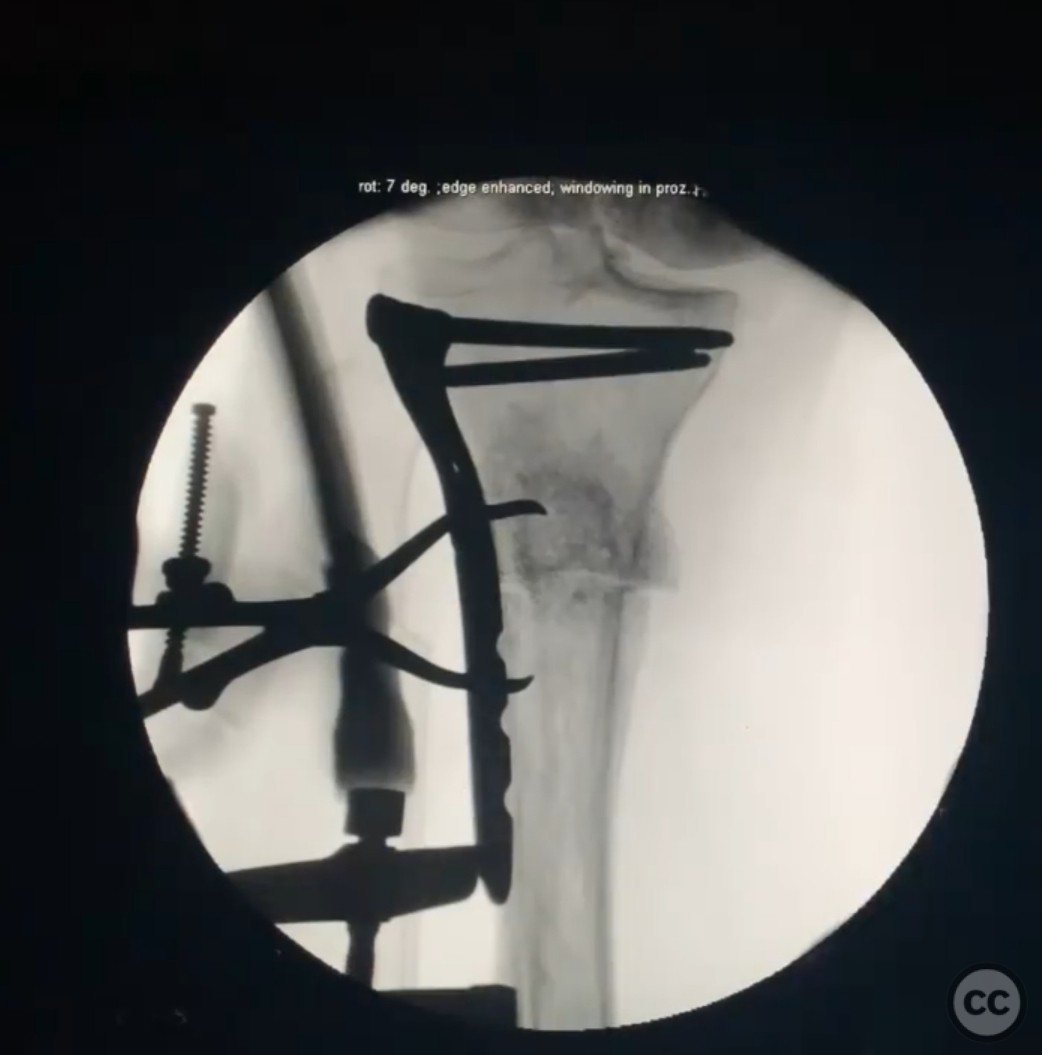
Planning remarks: The preoperative plan involved a staged surgical approach. Initially, fixation of the medial femoral condyle fracture was planned using a buttress plate and lag screw technique. Following successful healing and optimization of the patient's medical condition, a closing wedge osteotomy was planned to correct the proximal tibial malunion. The osteotomy aimed for a 17-degree correction with a 10mm wedge on the lateral cortex, addressing both varus and procurvatum deformities.
Surgical Discussion
Patient positioning: Supine positioning was utilized for the initial procedure, with appropriate padding to accommodate the patient's previous hindfoot fusion and ensure comfort during surgery.
Anatomical surgical approach: A lateral parapatellar approach was employed for the fixation of the medial femoral condyle fracture. The incision was made longitudinally along the lateral aspect of the knee, extending distally to expose the lateral femoral condyle. Subperiosteal dissection was performed to access the fracture site, allowing for reduction and fixation with a buttress plate and lag screw.
Operative remarks:The surgeon noted that the patient's bone quality was significantly compromised due to chronic steroid use, necessitating careful handling during fixation. Postoperatively, the patient demonstrated excellent healing of both the surgical wound and fracture site, achieving normal knee motion at three months. For the subsequent osteotomy, a slightly eccentric wedge was utilized to address procurvatum while minimizing height loss. The lateral tensioned plate provided compression across the osteotomy site, facilitating union.
Postoperative protocol: Postoperative rehabilitation included early mobilization with protected weight-bearing as tolerated. Range of motion exercises were initiated immediately to maintain knee flexibility, progressing to strengthening exercises as healing permitted.
Follow up: Not specified.
Orthopaedic implants used: Buttress plate, lag screw, tensioned lateral plate for osteotomy fixation.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities
















Article viewed 166 times
18 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). From Failure to Function: Staged Correction of Varus-Procurvatum Malunion and Medial Femoral Condyle Fracture in a Steroid-Dependent Patient". Journal of Orthopaedic Surgery and Traumatology. Case Report 40863464 Published Online Jul 18 2025.