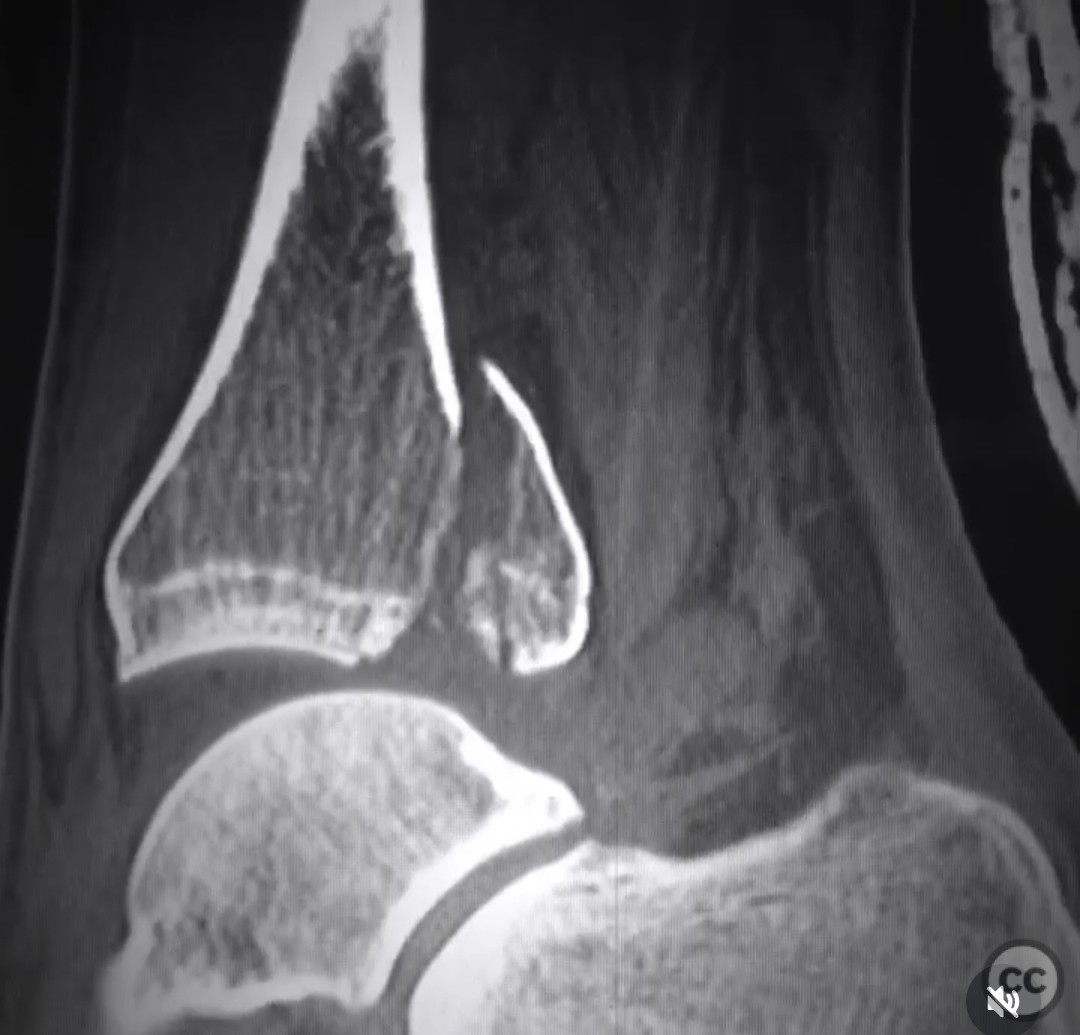
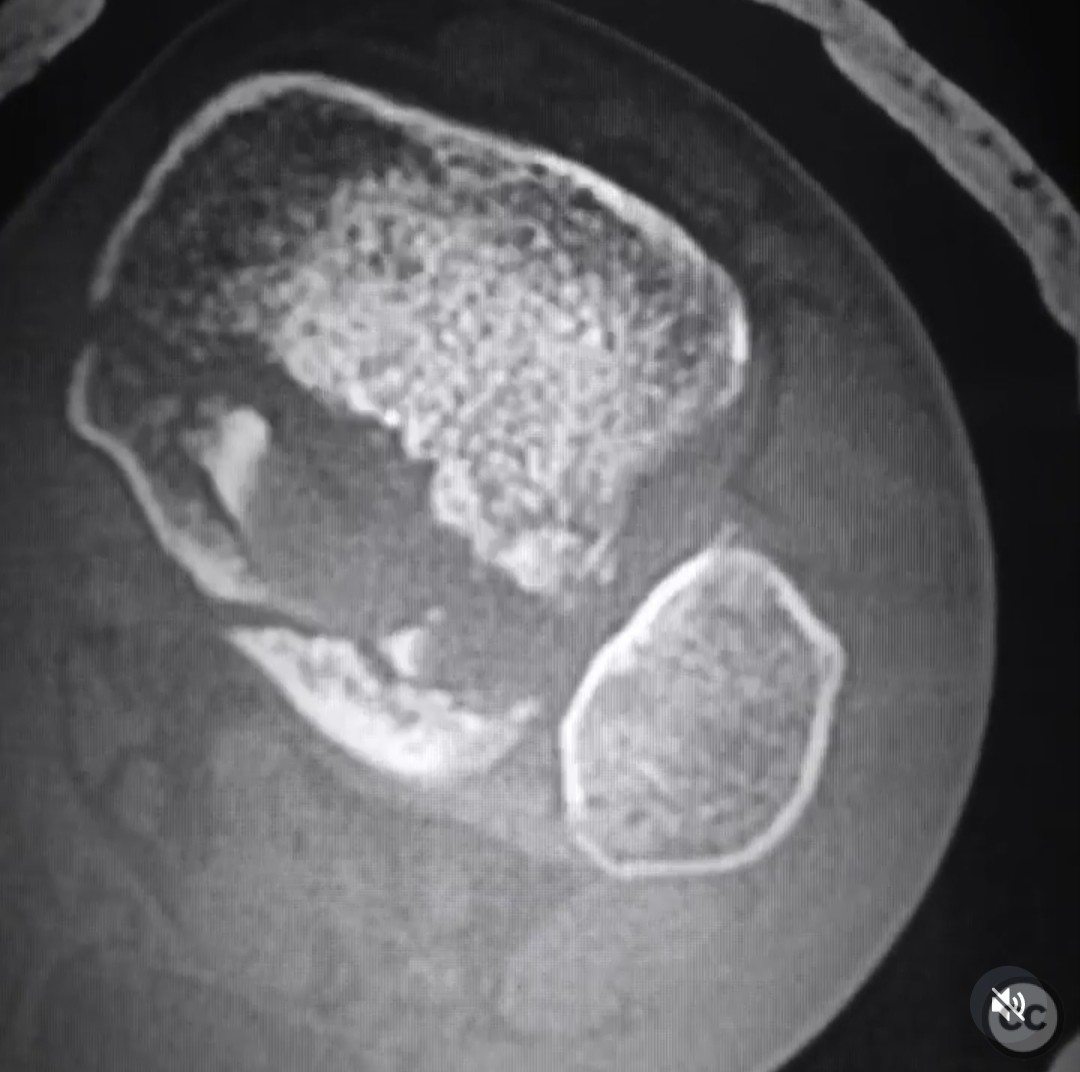
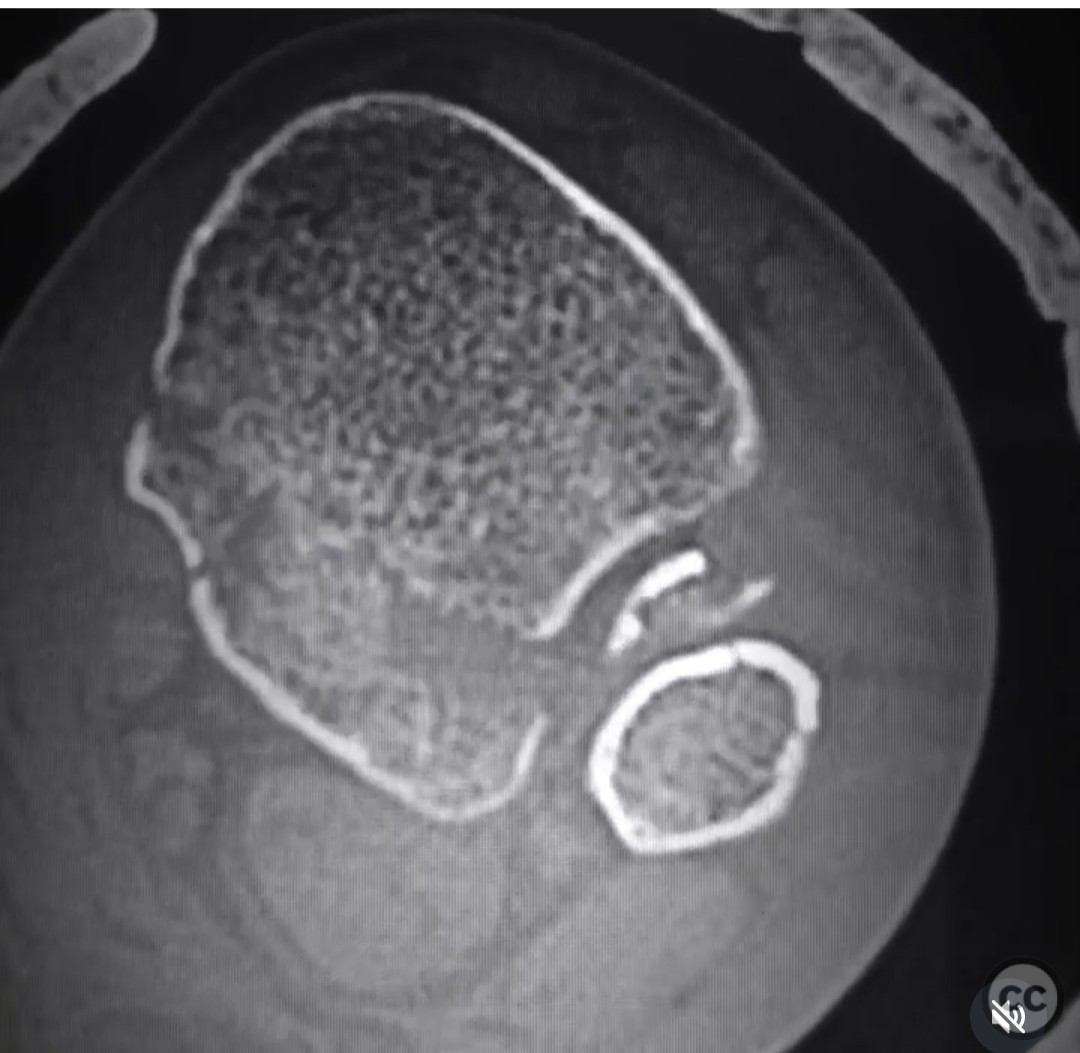
Trimalleolar Ankle Fracture Dislocation with Posterior Joint Impaction
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: A 34-year-old male sustained a trimalleolar ankle fracture dislocation while landing awkwardly during a basketball game. Initial radiographs and CT imaging revealed significant articular impaction, suggesting a prognosis akin to a pilon fracture. The injury was closed with no neurovascular compromise noted.
Preoperative Plan
Planning remarks: The preoperative plan involved a dual approach to address the posterior joint impaction. A posteromedial and posterolateral approach were planned to facilitate reduction and fixation of the posterior malleolus. Initial reduction of the fibula was prioritized to aid in the subsequent reduction of the posterior malleolus.
Surgical Discussion
Patient positioning: The patient was initially positioned prone to allow access to the posterior aspect of the ankle joint. This positioning facilitated the posteromedial and posterolateral approaches for reduction and fixation of the posterior malleolus.
Anatomical surgical approach: A posteromedial approach was made by incising along the medial border of the Achilles tendon, retracting it laterally to expose the posterior aspect of the tibia. A separate posterolateral approach was performed by incising along the lateral border of the Achilles tendon, retracting it medially to access the fibula and lateral aspect of the posterior tibia. The fibula was reduced and temporarily held with Kirschner wires. The articular surface was disimpacted, bone grafted, and temporarily held with wires before applying a buttress plate to each fragment through their respective approaches.
Operative remarks:The surgeon noted that reducing the fibula first and holding it with wires facilitated the reduction of the posterior malleolus. The fibula was not plated initially to avoid obstructing radiographic visualization during posterior malleolus reduction. After addressing the posterior elements, the patient was repositioned supine to address the small, comminuted medial malleolus fracture, which was fixed using a separate medial approach.
Postoperative protocol: Postoperatively, the patient was placed in a splint with non-weight bearing status for 6 weeks. Progressive weight bearing was initiated at 6 weeks, with full weight bearing anticipated by 10-12 weeks post-surgery.
Follow up: Not specified
Orthopaedic implants used: Buttress plates, Kirschner wires, bone graft
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities


Article viewed 197 times
28 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Trimalleolar Ankle Fracture Dislocation with Posterior Joint Impaction. Journal of Orthopaedic Surgery and Traumatology. Case Report 36200773 Published Online Jul 28 2025.