Posterior Wall and Transverse Acetabular Fracture-Dislocation with Medial Wall Involvement
Score and Comment on this Case
Clinical Details
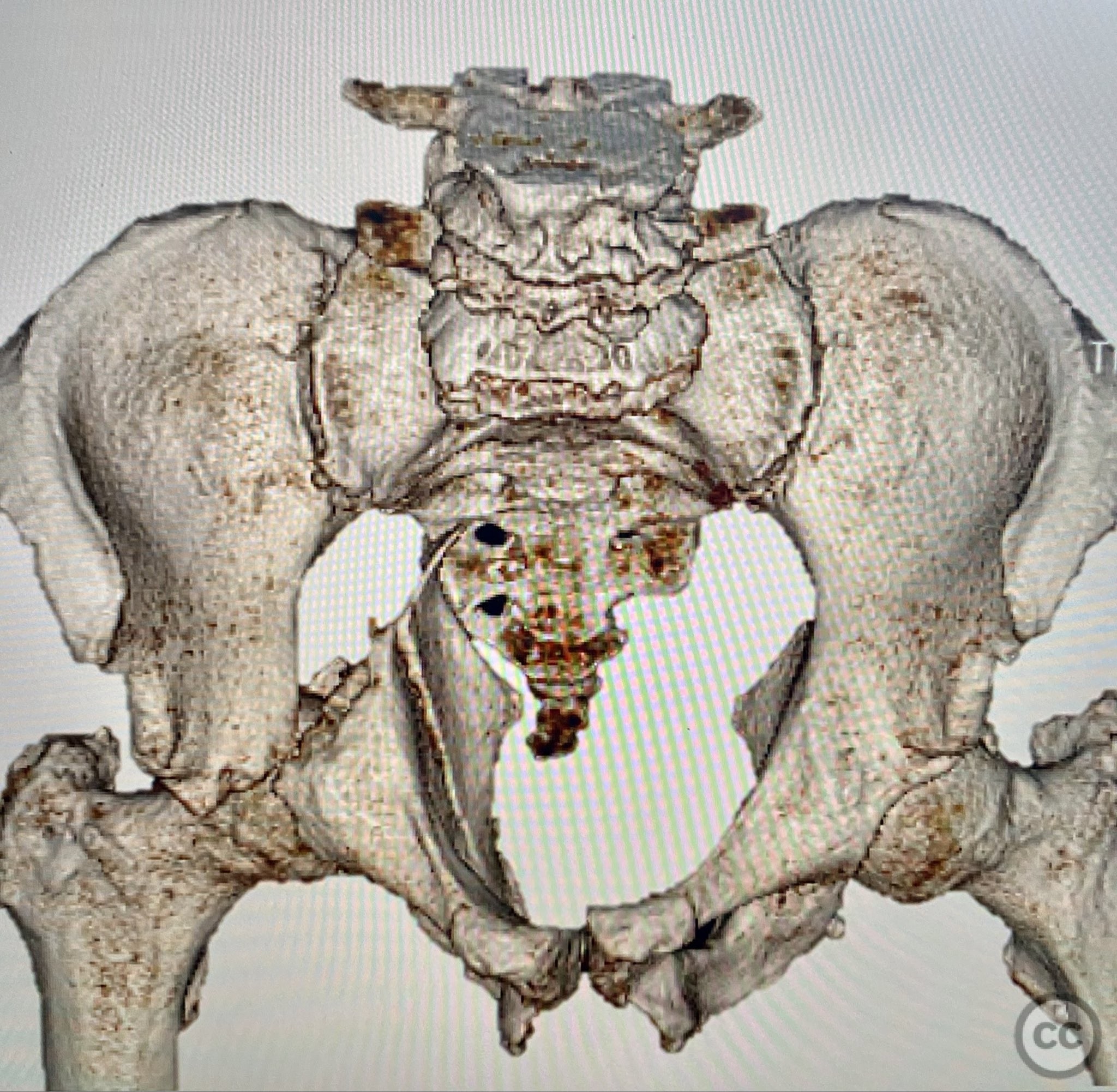
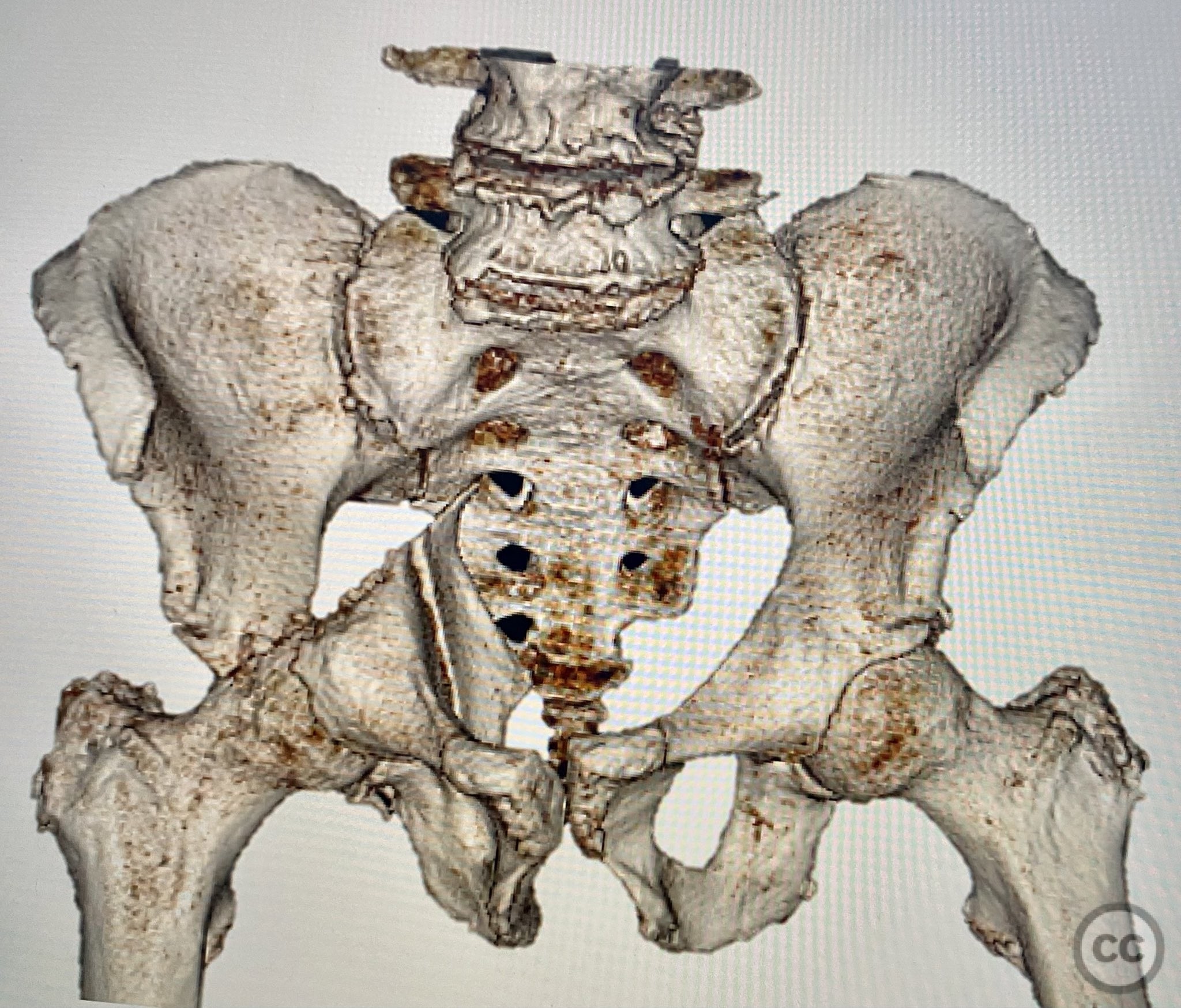
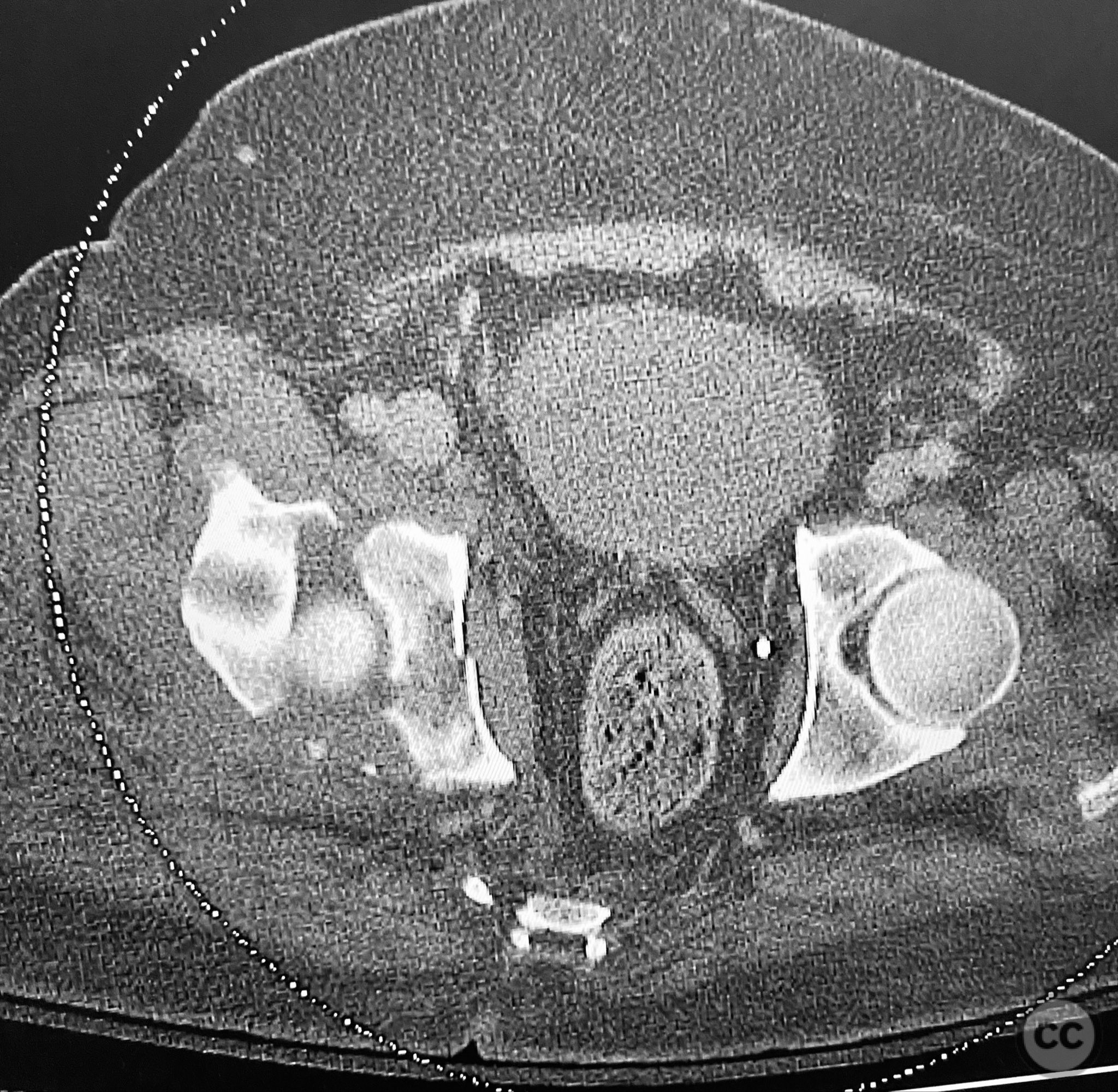
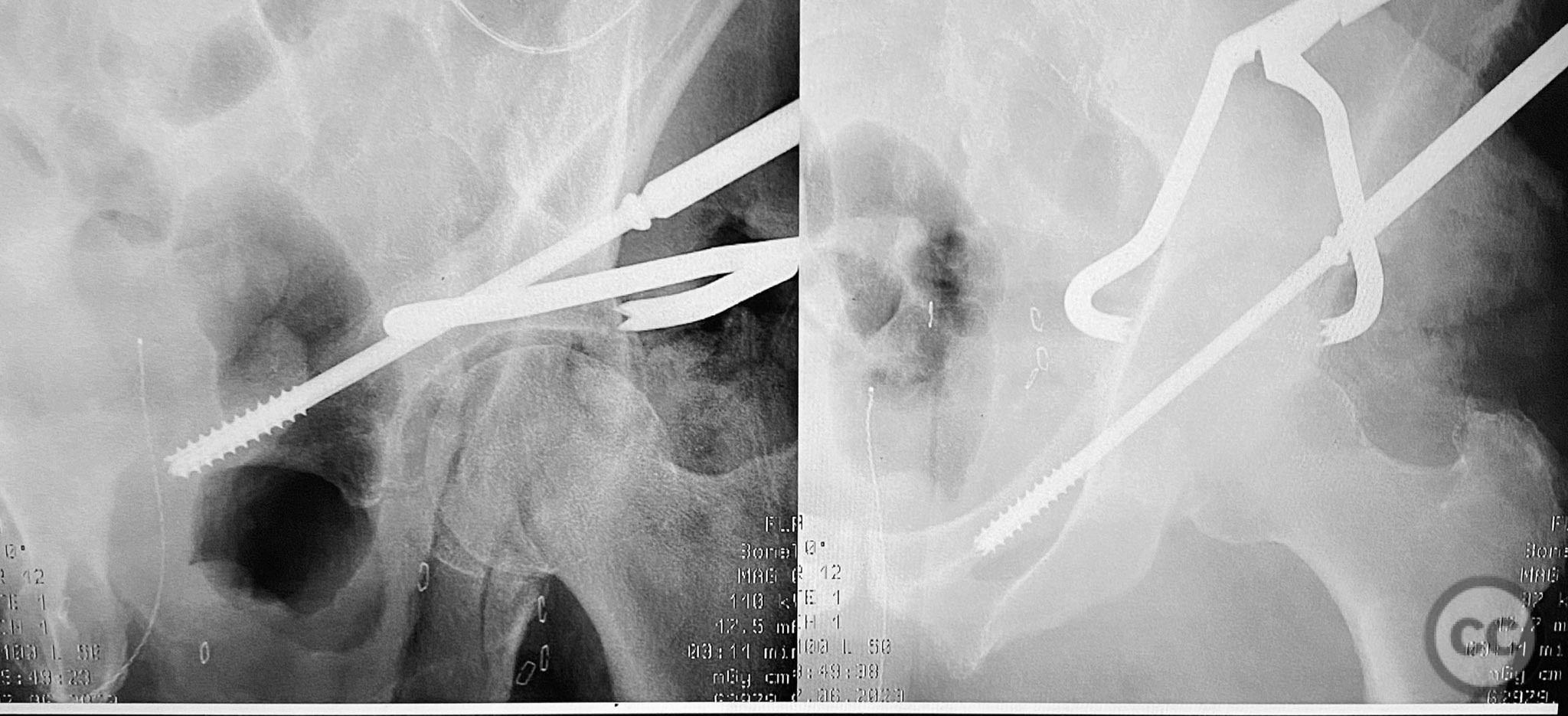
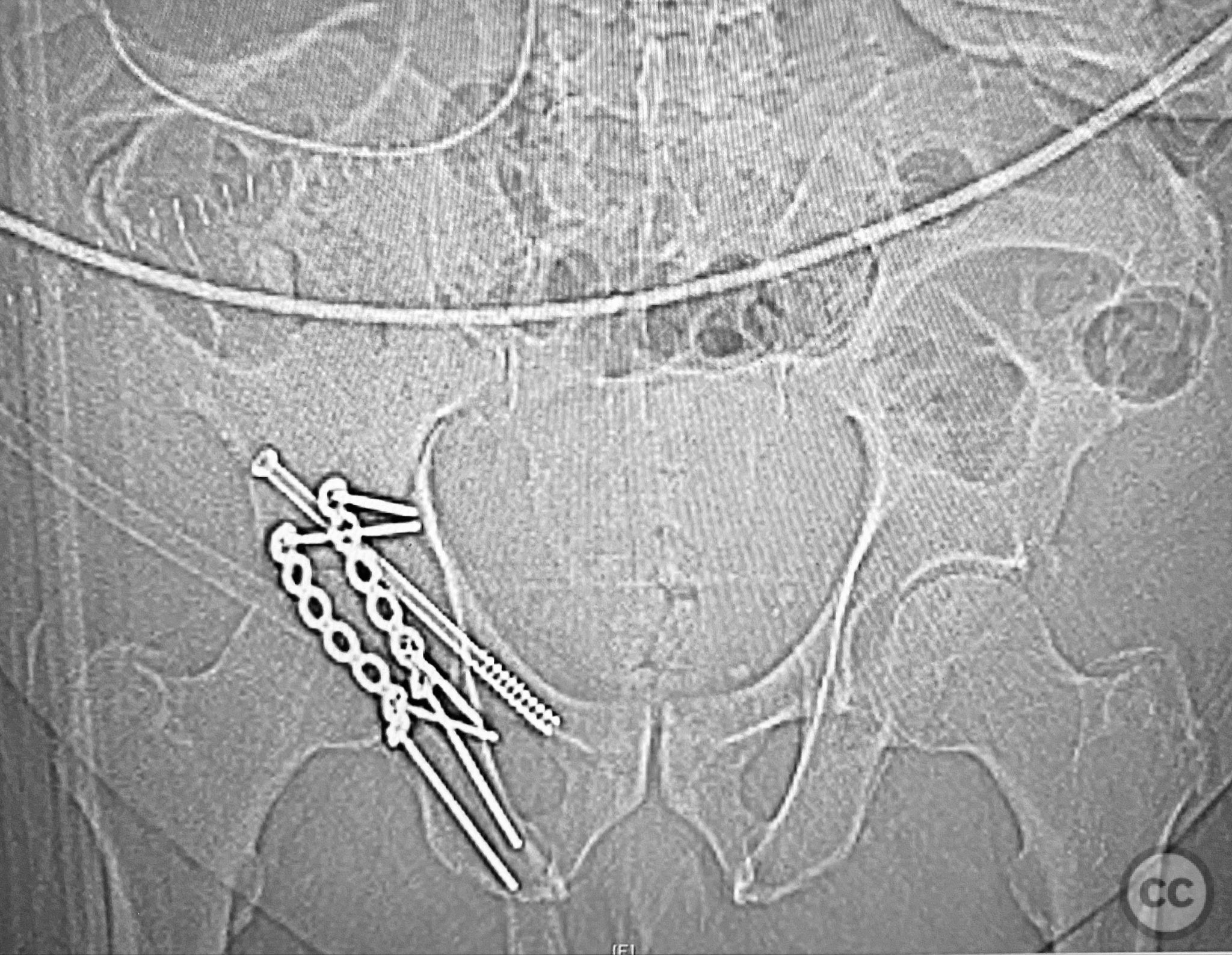
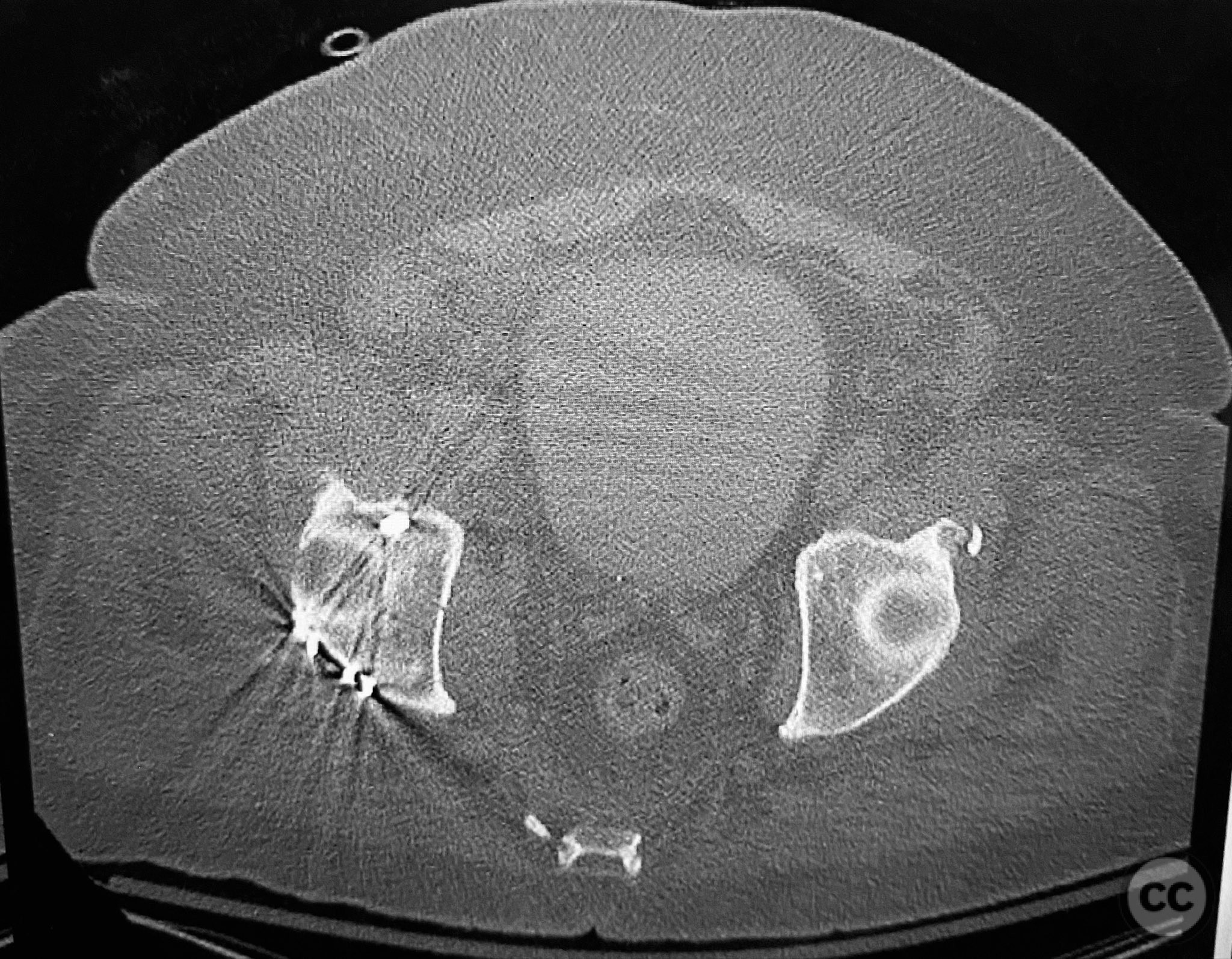
Clinical and radiological findings: A 79-year-old male sustained a high-energy injury in a motor vehicle collision, resulting in a complex acetabular fracture-dislocation. Radiographs and computed tomography demonstrated a posterior wall and transverse acetabular fracture (AO/OTA 62-B1.3), with the posterior wall fragments displaying an atypical caudal hinge configuration. The medial wall fragment was non-articular. Axial imaging revealed an impacted osteochondral fragment obstructing reduction, as well as disruption of the capsular structures adjacent to the intact articular segment. The obturator internus tendon appeared taut but intact, with no evidence of sciatic nerve impingement or superior gluteal neurovascular compromise.
Preoperative Plan
Planning remarks: The preoperative plan included open reduction and internal fixation via a Kocher-Langenbeck approach in the prone position. The strategy entailed removal of the impacted intra-articular fragment, anatomic reduction and provisional fixation of the transverse component, reduction and fixation of the posterior wall, bone grafting and reduction of the impacted articular segment via the medial wall window, and definitive fixation of the medial wall. Capsular repair was planned prior to closure.
Surgical Discussion
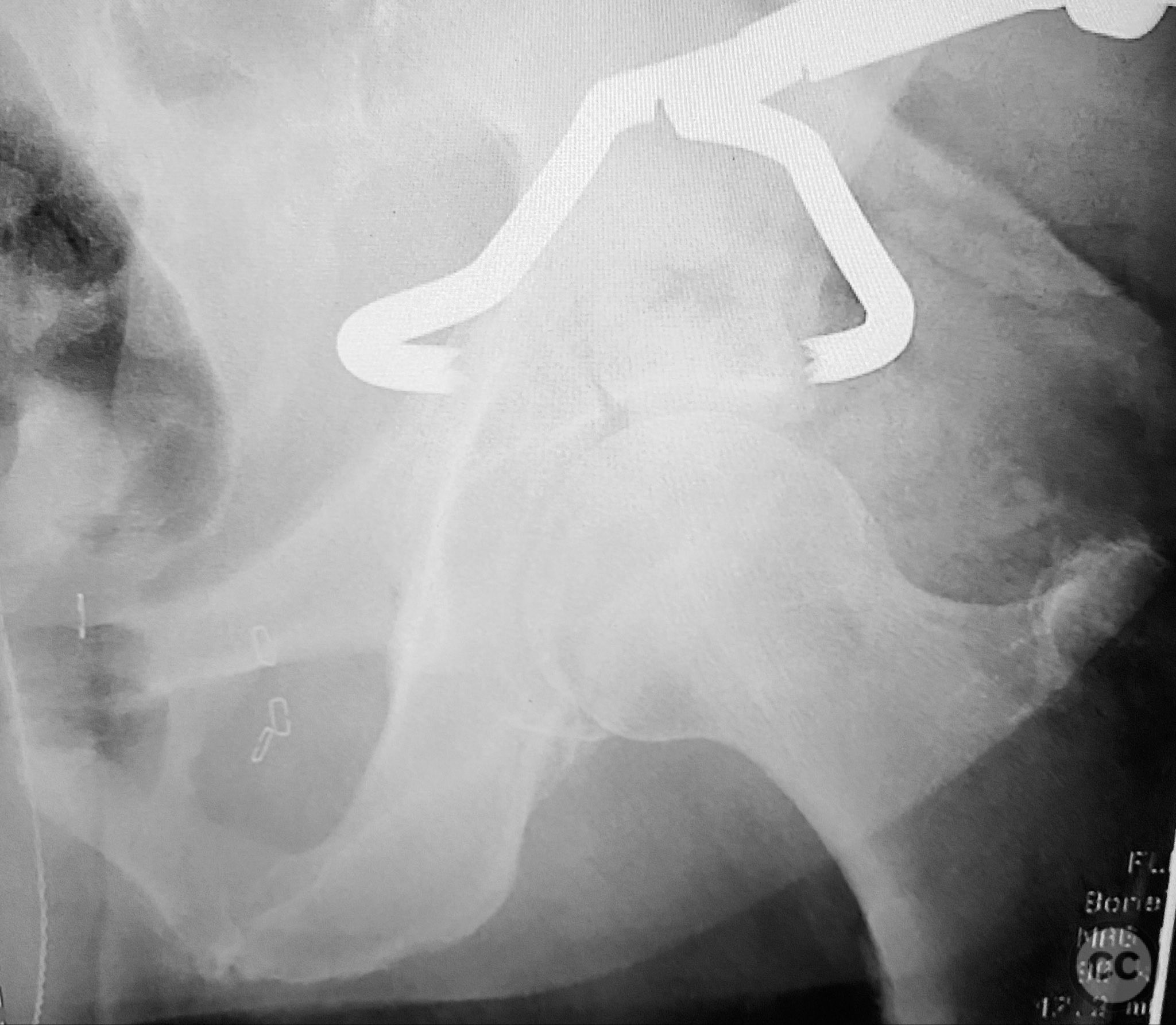
Patient positioning: The patient was positioned prone on a radiolucent table, with appropriate padding and supports to facilitate posterior pelvic access and fluoroscopic imaging.
Anatomical surgical approach: A standard Kocher-Langenbeck approach was performed, incising through the gluteal fascia and splitting the fibers of the gluteus maximus. The short external rotators were identified and protected, with subperiosteal dissection exposing the posterior column and wall of the acetabulum. The sciatic nerve was identified and mobilized laterally. The posterior capsule was found disrupted adjacent to the intact articular surface. The impacted osteochondral fragment was extracted from the joint space. The transverse fracture plane was debrided and reduced using clamps, with a greater trochanteric bone hook employed to manipulate the femoral head beneath the acetabular dome during reduction. Provisional fixation was achieved with a percutaneous lag screw across the transverse component. The peripheral posterior wall fragment was anatomically reduced and stabilized with a contoured plate. The medial wall defect provided access for reduction of the impacted articular segment, which was bone grafted prior to reduction and plating of the medial wall. Capsular tissues were repaired with nonabsorbable sutures prior to layered wound closure.
Operative remarks:The posterior wall fragments exhibited an unusual caudal hinge morphology, necessitating careful mobilization to avoid propagation or comminution. Removal of the impacted intra-articular fragment was essential to achieve concentric reduction of the femoral head within the acetabular dome. Use of a greater trochanteric bone hook facilitated precise control of femoral head position during reduction maneuvers. The medial wall fragment, though non-articular, allowed direct visualization and accurate reduction of the impacted osteochondral segment, which was supported with bone graft prior to definitive fixation. Repair of disrupted capsular tissues was performed to restore soft tissue integrity and potentially reduce postoperative instability.
Postoperative protocol: Postoperatively, toe-touch weight bearing was instituted for 8 weeks with active-assisted range of motion exercises initiated immediately. Hip flexion was limited to 90 degrees for 6 weeks to protect capsular repair. Abduction and external rotation were restricted during early rehabilitation. Progressive weight bearing commenced at 8 weeks based on radiographic evidence of healing.
Follow up: Not specified
Orthopaedic implants used: 3.5mm pelvic reconstruction plate (posterior wall), 3.5mm pelvic reconstruction plate (medial wall), percutaneous cannulated lag screw, cancellous bone graft
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities






Article viewed 116 times
12 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Posterior Wall and Transverse Acetabular Fracture-Dislocation with Medial Wall Involvement. Journal of Orthopaedic Surgery and Traumatology. Case Report 36137524 Published Online Sep 12 2025.