Complex Proximal Tibiofibular Joint Dislocation Associated with an Open Comminuted Diaphyseal Tibial Fracture
Score and Comment on this Case
Clinical Details
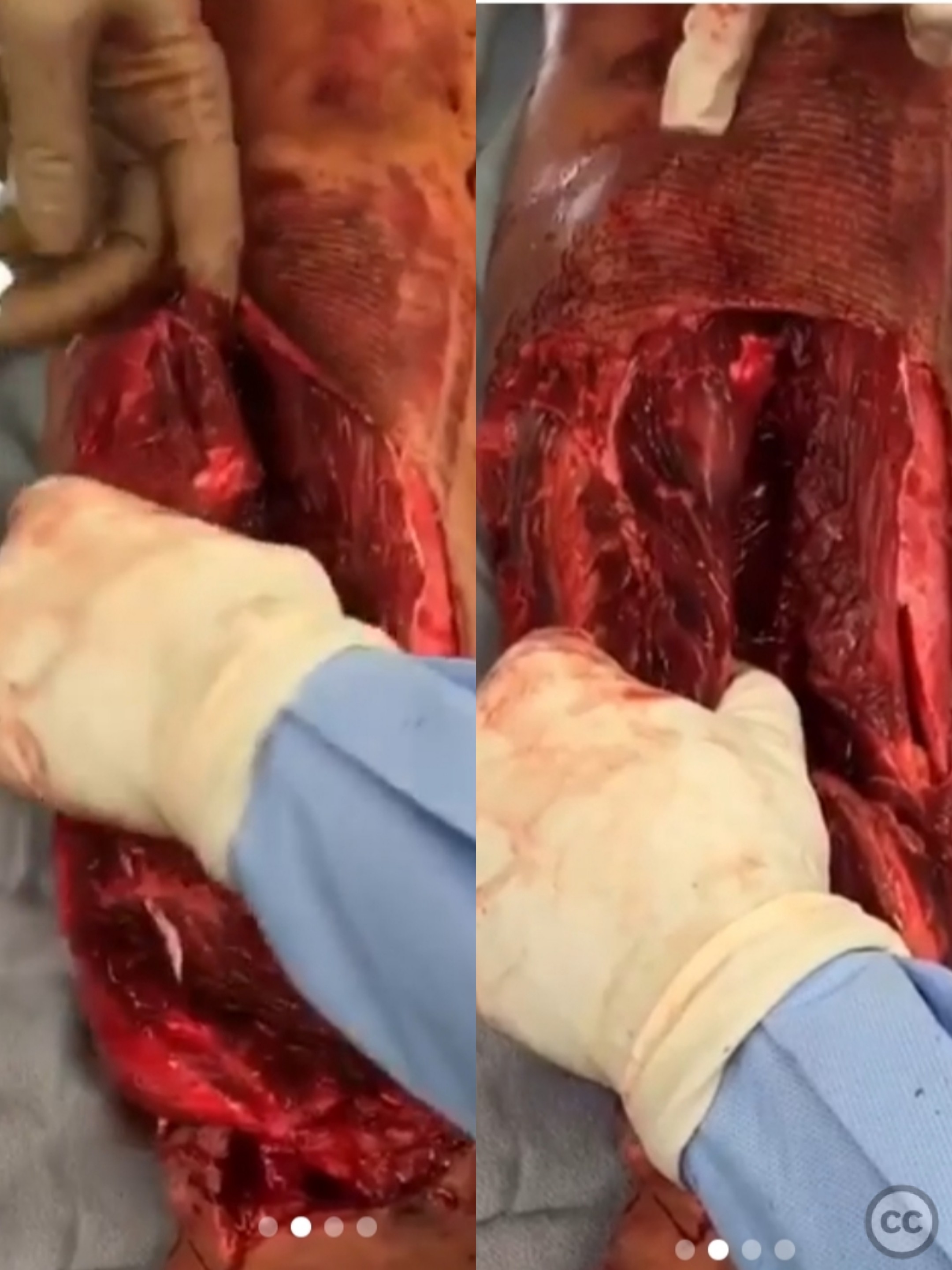
Clinical and radiological findings: A 32-year-old male was struck by a vehicle, resulting in a severe injury characterized by a comminuted diaphyseal tibia fracture and proximal fibula dislocation. The lateral compartment and proximal tibial segment were significantly displaced. Initial clinical examination revealed palpable posterior tibial pulse and retrograde dopplerable dorsalis pedis pulse, indicating well-perfused foot. The tibial nerve was intact despite the severe soft tissue injury.
Preoperative Plan
Planning remarks: The preoperative plan included thorough debridement of the soft tissue, followed by intramedullary nailing of both the tibia and fibula. Fixation of the proximal tibiofibular dislocation was also planned. A latissimus dorsi flap was scheduled for soft tissue coverage postoperatively.
Surgical Discussion
Patient positioning: Supine positioning on the operating table with appropriate padding to maintain limb alignment and facilitate surgical access.
Anatomical surgical approach: The existing open wound over the anterolateral aspect of the leg was extended as needed to access the tibial diaphysis and the dislocated proximal fibula. Subperiosteal dissection was carried out to expose the fracture site. The intercalary tibial fragment was utilized temporarily to assist in anatomical reduction during intramedullary nailing
Operative remarks:Completely devitalized segments of bone shouldn’t be discarded right away—they can still serve a critical role in achieving anatomical reduction. In this case, the intercalary tibial fragment, although devitalized, was temporarily used to facilitate anatomical alignment during intramedullary nailing and subsequently discarded. Once its role was complete, the segment was removed and the defect managed using the Masquelet technique. A polymethylmethacrylate (PMMA) spacer was placed to address the bone void, with plans for autografting at six weeks postoperatively. The proximal tibiofibular dislocation was also stabilized."
Postoperative protocol: Postoperative protocol included immobilization with limited weight-bearing on the affected limb. Progressive weight-bearing was anticipated following soft tissue healing and subsequent autografting.
Follow up: Not specified.
Orthopaedic implants used: Intramedullary nail for tibia and fibula, PMMA spacer, fixation devices for proximal tibiofibular dislocation.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










Article viewed 161 times
25 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Complex Proximal Tibiofibular Joint Dislocation Associated with an Open Comminuted Diaphyseal Tibial Fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 34176170 Published Online Jul 25 2025.