Posterior Wall Acetabular Fracture-Dislocation with Cranial Lateral Impaction and Failed Closed Reduction
Score and Comment on this Case
Clinical Details
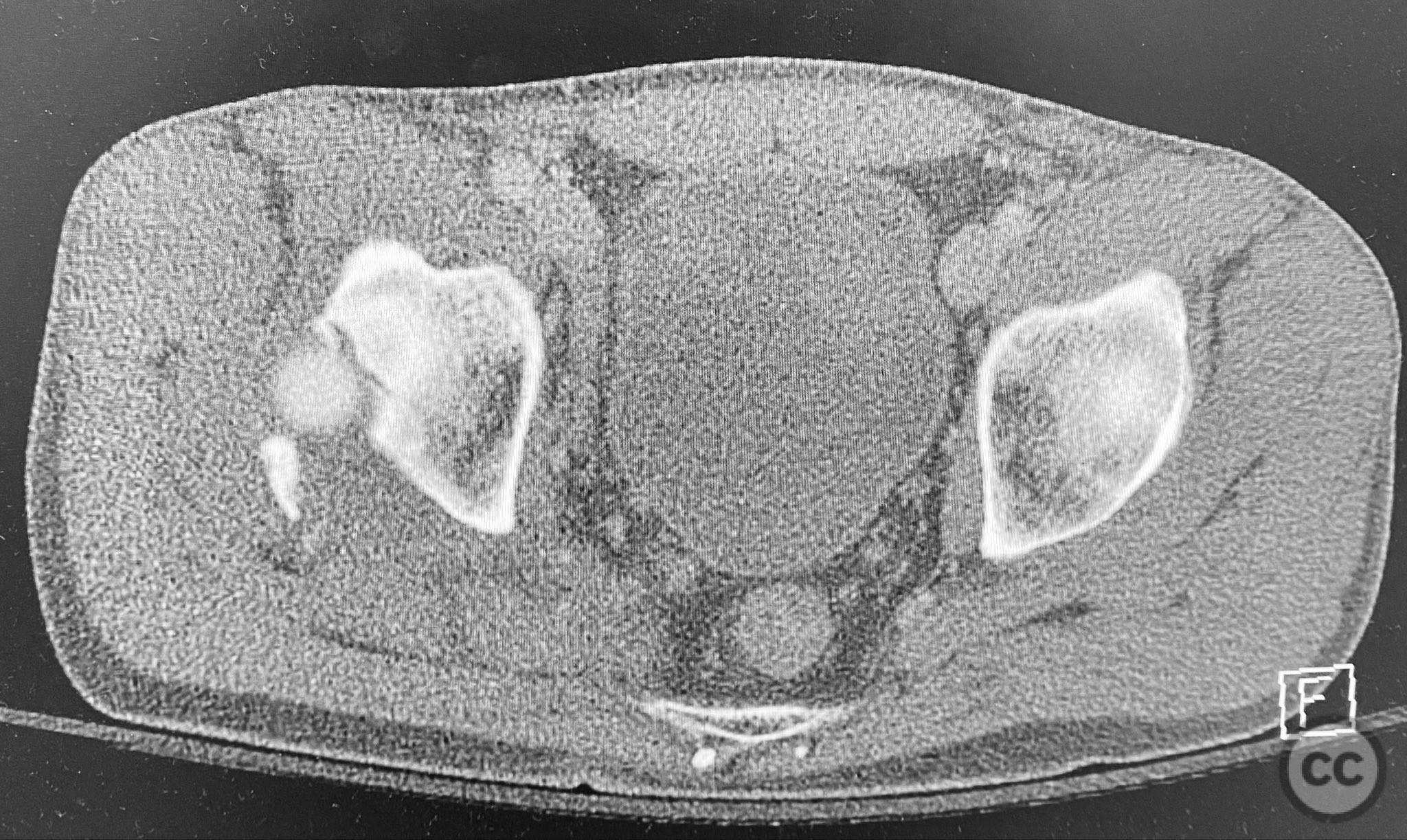
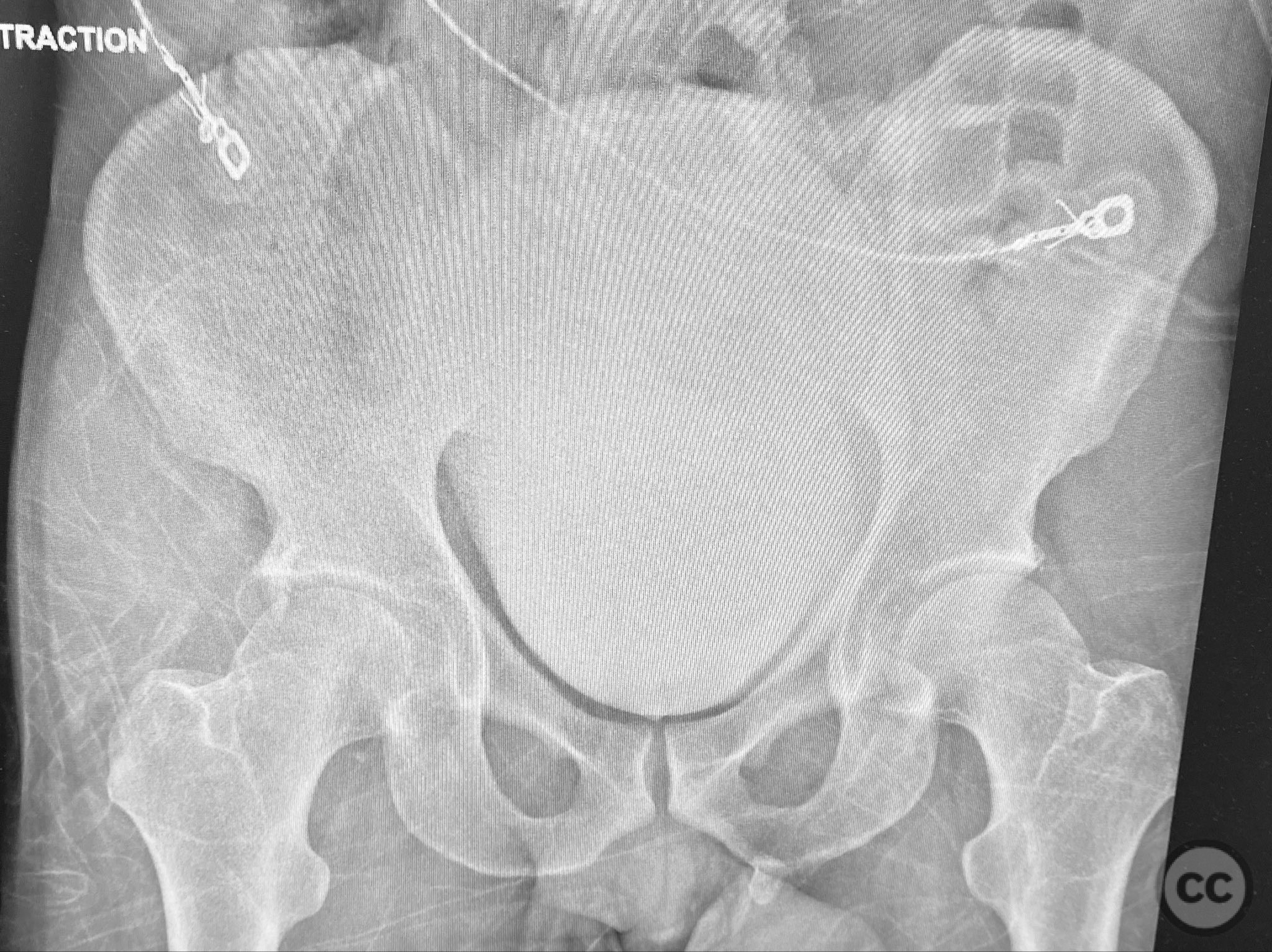
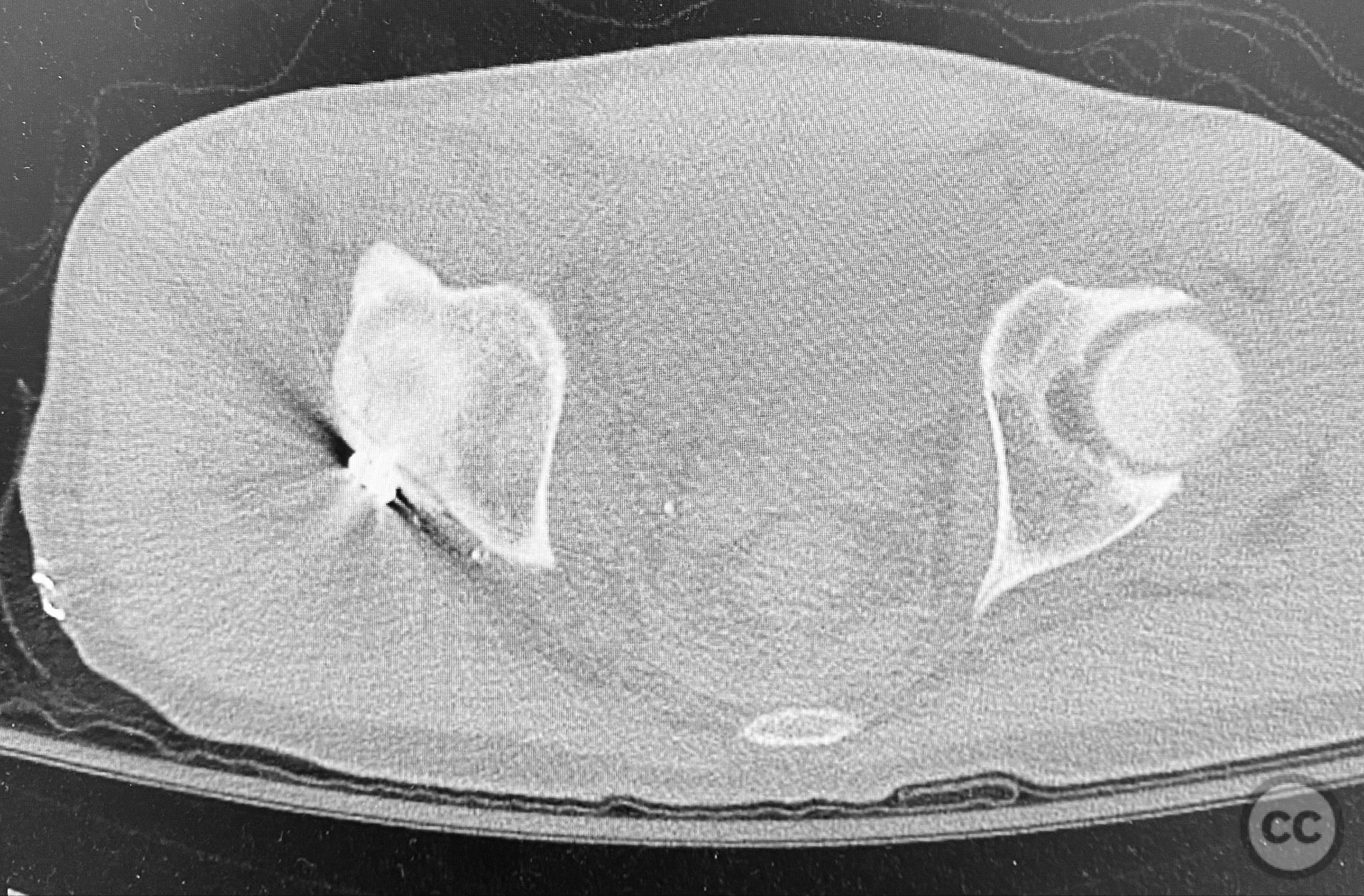
Clinical and radiological findings: A middle-aged patient sustained a posterior wall acetabular fracture-dislocation, as demonstrated on initial AP pelvic radiograph. The film revealed a sizeable posterior wall fragment, cranial lateral impaction of the acetabular dome, and subtle deformation of the femoral head contour. Neurovascular examination was performed, including assessment of distal pulses and sciatic nerve function. The ipsilateral knee and anterior chest were examined for associated injuries (including possible knee ligamentous injury and thoracic trauma). An initial attempt at closed reduction under sedation was unsuccessful.
Preoperative Plan
Planning remarks: The preoperative plan included advanced imaging with CT, including 3D surface renderings, to further delineate the extent of articular impaction, wall fragment size, and comminution. The plan was for open reduction and internal fixation via a posterior Kocher-Langenbeck approach in the prone position. Elevation of impacted articular segments was planned, with structural support using autologous bone graft harvested from the greater trochanter. Fragment-specific fixation was planned with a spring hook plate for the cranial wall fragment and a reconstruction plate for the main posterior wall fragment.
Surgical Discussion
Patient positioning: The patient was positioned prone on a radiolucent table, with all pressure points padded. Skeletal traction was maintained via a distal femoral K-wire and tensioning bow throughout the procedure.
Anatomical surgical approach: A standard Kocher-Langenbeck approach was utilized. A longitudinal incision was made centered over the greater trochanter, extending proximally and distally as required. The fascia lata was incised in line with the skin incision, and the gluteus maximus was split in the direction of its fibers. The short external rotators (piriformis, obturator internus, gemelli) were identified and retracted or released as necessary to expose the posterior column and wall of the acetabulum. The sciatic nerve was identified and protected throughout. The impacted articular surface was elevated using dedicated elevators, and the defect was filled with autologous corticocancellous bone graft harvested from the greater trochanter. The cranial wall fragment was reduced anatomically and secured with a spring hook plate. The main posterior wall fragment was then reduced and stabilized with a contoured reconstruction plate.
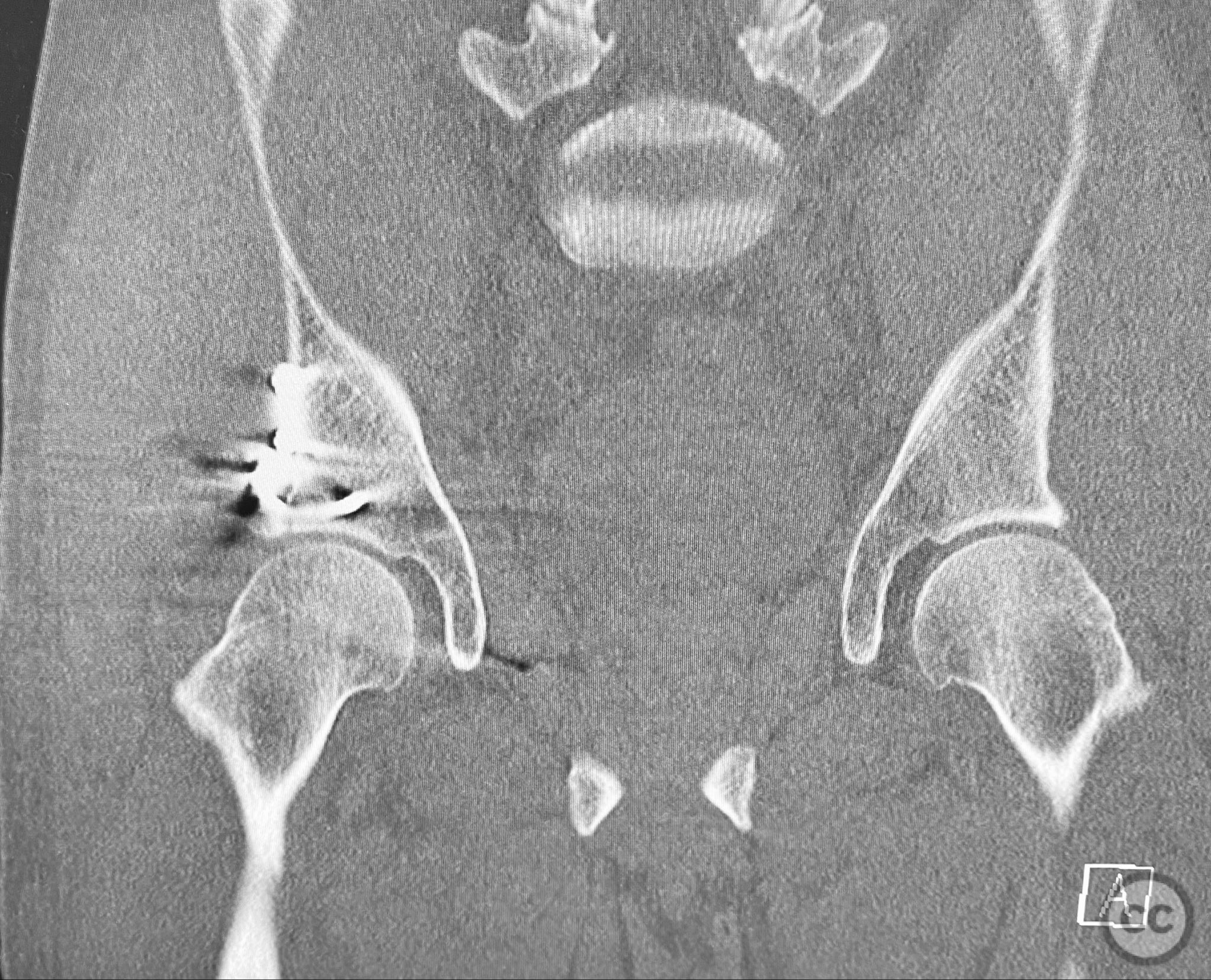
Operative remarks:The initial failed closed reduction likely resulted from interposed soft tissue or bony fragments, or inadequate sedation/muscle relaxation. Repeat reduction under improved conditions was successful prior to definitive fixation. 3D CT renderings provided enhanced visualization of impaction zones and comminution, facilitating preoperative planning for grafting and fragment-specific fixation. Intraoperatively, elevation of the impacted dome required careful manipulation to avoid further chondral injury. Use of a spring hook plate provided secure fixation of the cranial wall fragment, while the reconstruction plate supported the main wall fragment. Postoperative CT confirmed satisfactory reduction and implant positioning.
Postoperative protocol: Protected weight bearing (toe-touch or partial) is recommended for 6-8 weeks postoperatively, with progressive increase in weight bearing thereafter as radiographic healing permits. Early passive range of motion exercises are initiated to minimize joint stiffness.
Follow up: Not specified
Orthopaedic implants used: Spring hook plate; 3.5mm reconstruction plate; autologous trochanteric bone graft; distal femoral K-wire (for skeletal traction)
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities



.jpg)






Article viewed 455 times
12 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Posterior Wall Acetabular Fracture-Dislocation with Cranial Lateral Impaction and Failed Closed Reduction. Journal of Orthopaedic Surgery and Traumatology. Case Report 3403939 Published Online Sep 12 2025.