Symptomatic Nonunion of Clavicle Fracture with Synovial Pseudarthrosis in an Active Male
Score and Comment on this Case
Clinical Details
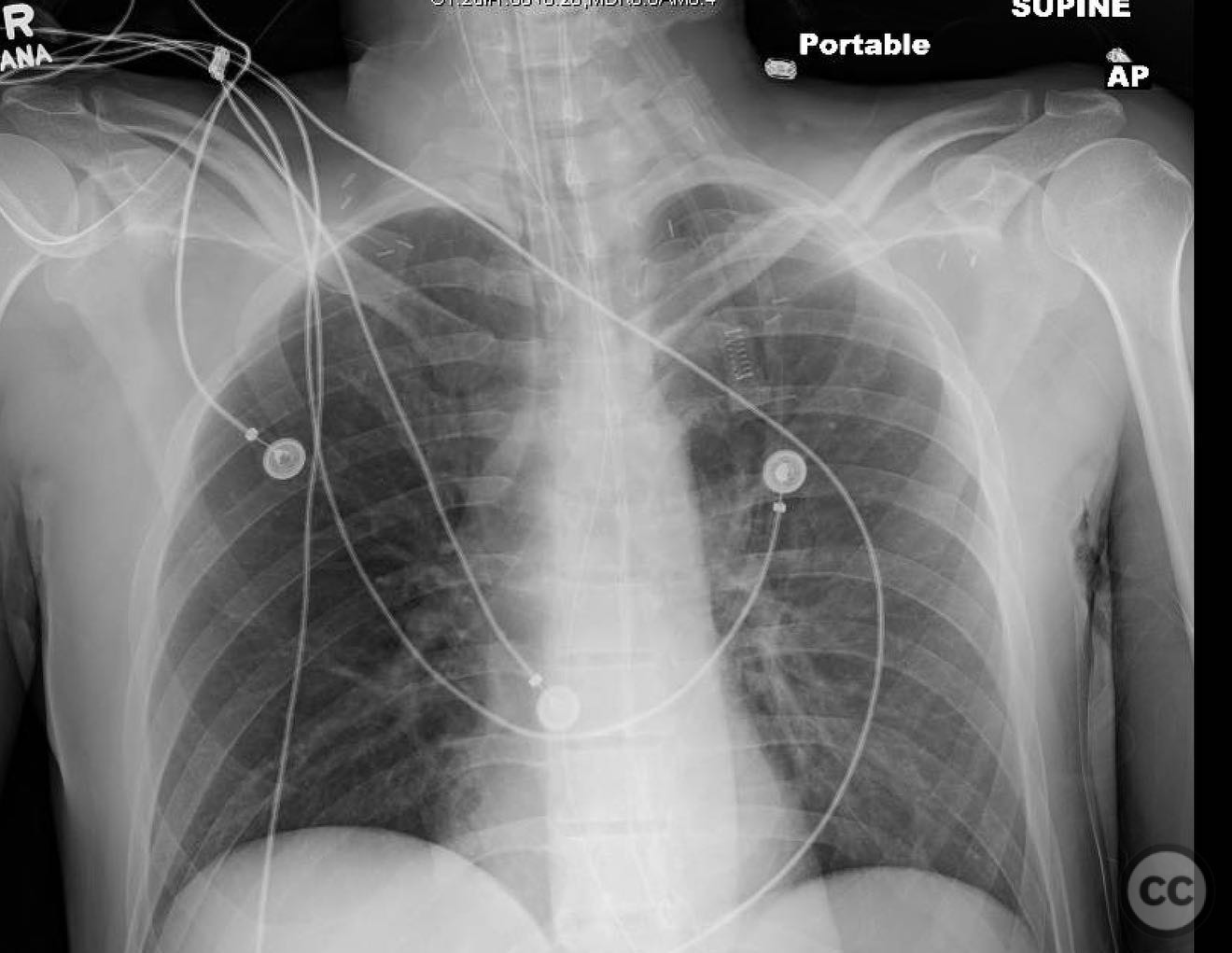
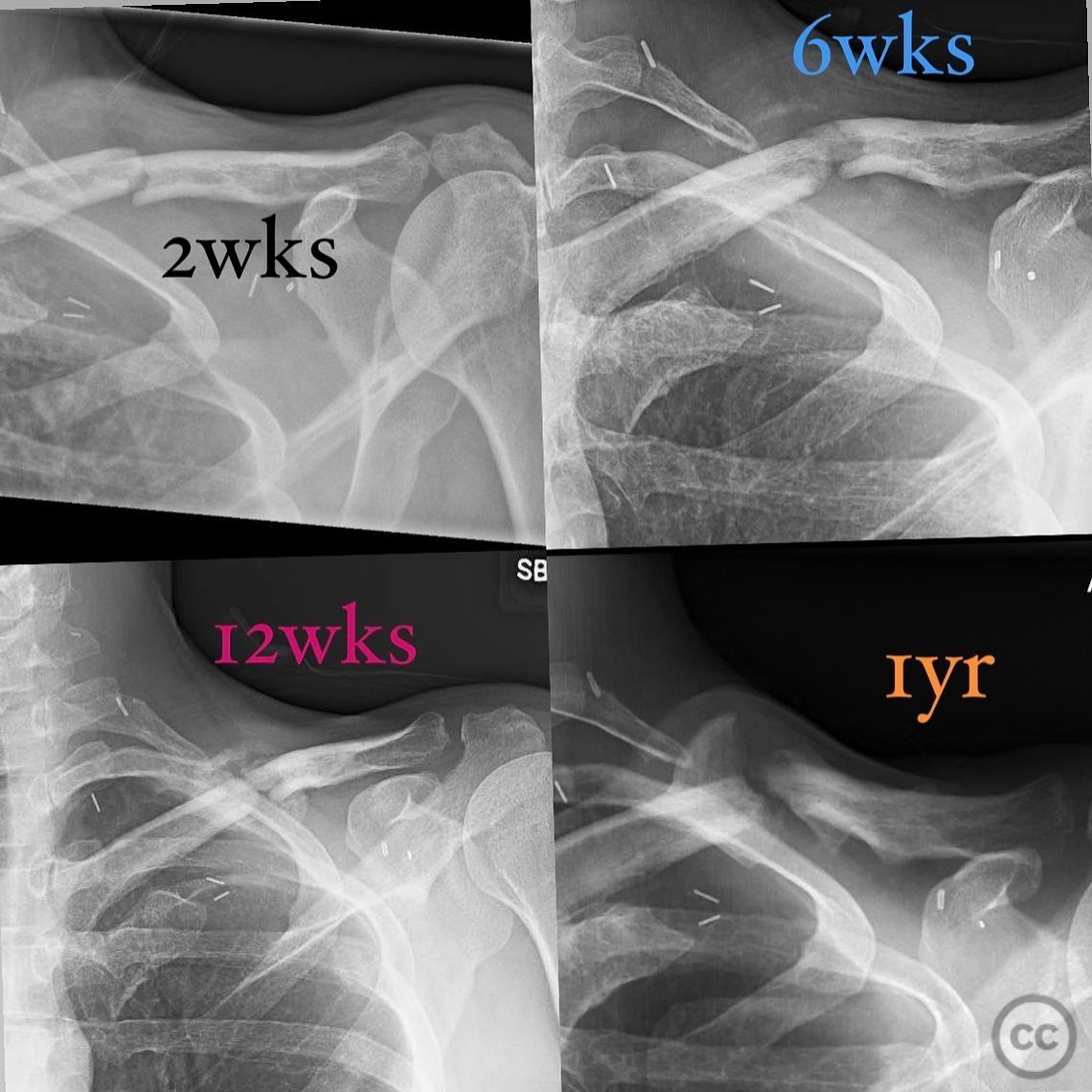
Clinical and radiological findings: A 42-year-old healthy, active male presented with a symptomatic nonunion of the clavicle one year post-injury. The patient initially sustained a closed, minimally displaced clavicle fracture from a mountain biking accident. Initial radiographs showed no significant shortening and approximately 25% displacement. Follow-up radiographs at 6 and 12 weeks demonstrated maintained alignment and callus formation. Despite these findings, the patient developed a symptomatic nonunion characterized by gross motion and pain, although shoulder motion remained normal. The patient had a history of first rib resection and scalenectomy for thoracic outlet syndrome (TOS). Nonunion labs were normal.
Preoperative Plan
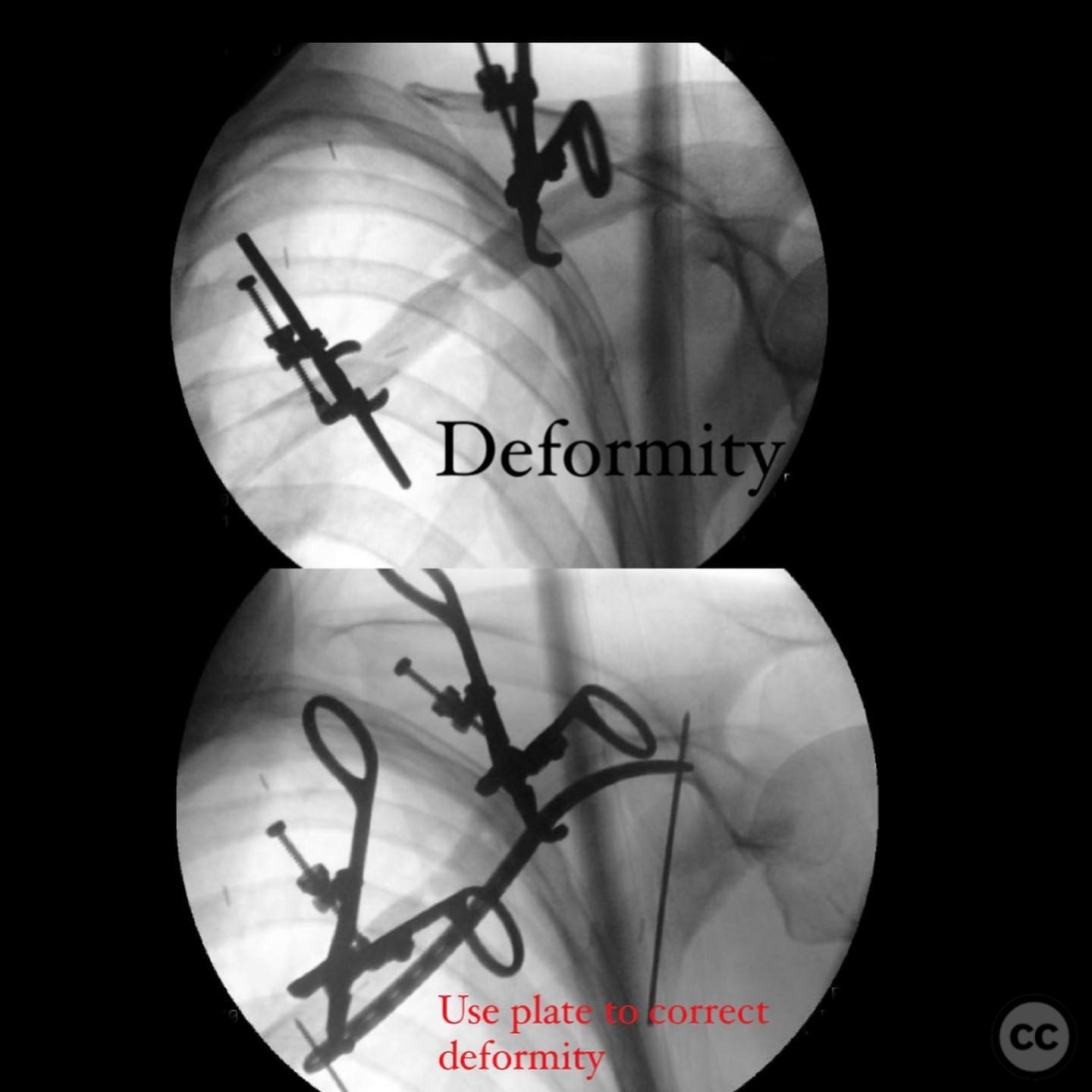
Planning remarks: The preoperative plan involved addressing the synovial pseudarthrosis by re-establishing the medullary canals, debriding all synovial and fibrous tissue, burring sclerotic bone to expose healthy bleeding bone, correcting any deformity, and using autograft for bone loss. Stable fixation was planned to allow early motion and promote union. The surgical approach was planned to be an open reduction with internal fixation using a precontoured plate and orthogonal plating for added torsional stability.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table with the affected shoulder elevated and supported to allow optimal access to the clavicle.
Anatomical surgical approach: A direct superior approach to the clavicle was utilized. An incision was made over the clavicle, and subperiosteal dissection was performed to expose the fracture site. The synovial and fibrous tissue was meticulously debrided, and the sclerotic bone ends were burred to reveal healthy bleeding bone. The medullary canals were re-established, and a cortico-cancellous autograft from the gluteal pillar was fashioned into a wedge to fill the anterior defect.
Operative remarks:The surgeon noted that the synovial pseudarthrosis presented unique challenges due to the encapsulation and synovial fluid presence at the nonunion site. The bone ends were sclerotic with obliterated medullary canals, necessitating thorough debridement and preparation for grafting. Orthogonal plating provided additional torsional stability, crucial for promoting union in this case.
Postoperative protocol: Postoperatively, the patient was advised to engage in early passive range of motion exercises to maintain shoulder mobility while avoiding excessive stress on the repair site. Weight-bearing activities were restricted until radiographic evidence of union was observed.
Follow up: Not specified.
Orthopaedic implants used: Precontoured clavicle plate, orthogonal plating system, cortico-cancellous autograft from the gluteal pillar.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










Article viewed 185 times
13 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Symptomatic Nonunion of Clavicle Fracture with Synovial Pseudarthrosis in an Active Male. Journal of Orthopaedic Surgery and Traumatology. Case Report 33776072 Published Online Jul 13 2025.