Sequential Anterior and Posterior ORIF for Combined SP and SI/Sacral Injuries with Open Posterior Wound
Score and Comment on this Case
Clinical Details
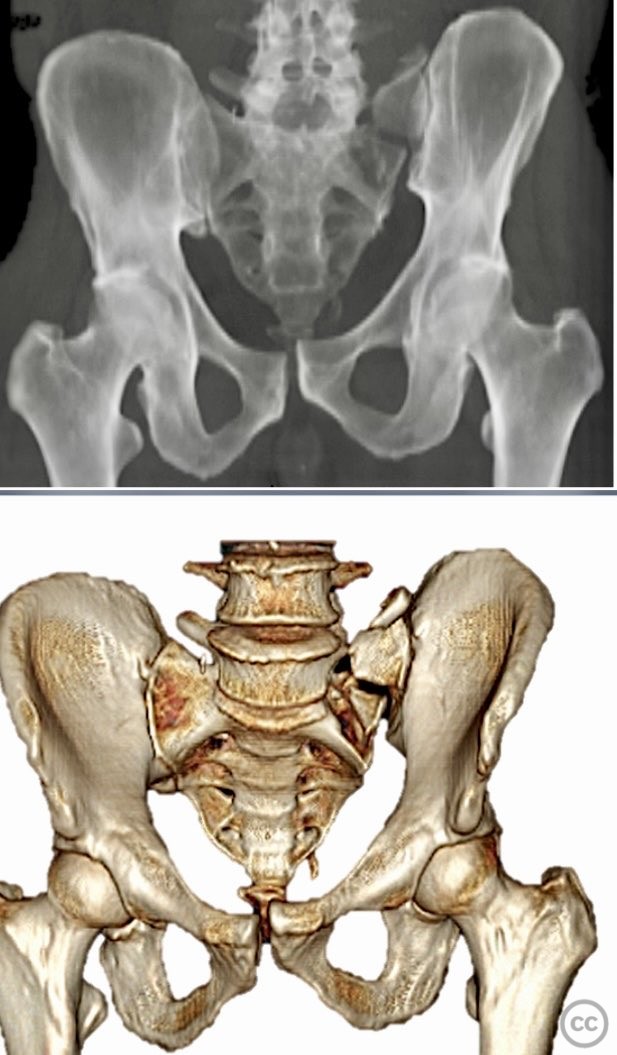
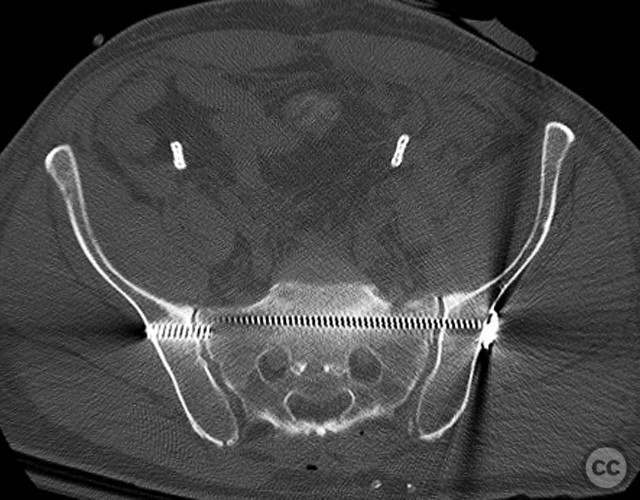
Clinical and radiological findings: Middle-aged male involved in a motor vehicle accident sustained a complete symphysis pubis (SP) disruption and left sacroiliac (SI)/sacral combination fracture-dislocation (AO/OTA 61-C1.3). The patient presented with an open traumatic posterior pelvic wound. Initial assessment revealed hemodynamic instability requiring urgent laparotomy and subsequent angioembolization for pelvic hemorrhage. Axial CT imaging demonstrated significant displacement of the anterior and posterior pelvic ring, with embolic coils visible post-intervention.
Preoperative Plan
Planning remarks: The preoperative plan included staged fixation: initial supine positioning for low midline exposure and open reduction internal fixation (ORIF) of the pubic symphysis, followed by prone repositioning for irrigation and debridement (I&D) of the open posterior wound and stabilization of the posterior pelvic ring via iliosacral screw fixation under fluoroscopic guidance.
Surgical Discussion
Patient positioning: The patient was first positioned supine for anterior pelvic exposure and fixation, then repositioned prone for posterior wound management and fixation.
Anatomical surgical approach: Anteriorly, a low midline infraumbilical incision was made to expose the symphysis pubis, with subperiosteal dissection of the rectus sheath and direct visualization of the disrupted symphysis. Posteriorly, a longitudinal midline approach over the sacrum was utilized, incorporating the traumatic wound for I&D. Deep dissection allowed access to the sacral ala and SI joint. A tenaculum clamp was applied percutaneously to achieve reduction of the sacral/SI fracture-dislocation. Iliosacral screws were inserted percutaneously under fluoroscopic control across the SI joint into S1.
Operative remarks:The sequence of anterior then posterior fixation allowed unimpeded access to both injury sites. The use of a tenaculum clamp facilitated reduction of the complex posterior injury. No technical interference was encountered between anterior plate fixation and subsequent posterior iliosacral screw placement. The presence of embolic coils did not impede surgical access or reduction maneuvers.
Postoperative protocol: Early mobilization with protected weight bearing was initiated. Supine positioning was maintained for 48 hours postoperatively, followed by gradual progression to sitting and standing as tolerated. Non-weight bearing on the affected side was maintained for 6 weeks, with progression to partial weight bearing thereafter based on radiographic healing.
Follow up: Not specified
Orthopaedic implants used: 3.5 mm anterior symphyseal plate, cannulated iliosacral screws
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities





Article viewed 147 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Sequential Anterior and Posterior ORIF for Combined SP and SI/Sacral Injuries with Open Posterior Wound. Journal of Orthopaedic Surgery and Traumatology. Case Report 30263982 Published Online Sep 11 2025.