Hyperextension Varus Bicondylar Tibial Plateau Fracture in a Diabetic Patient with Peripheral Neuropathy
Score and Comment on this Case
Clinical Details
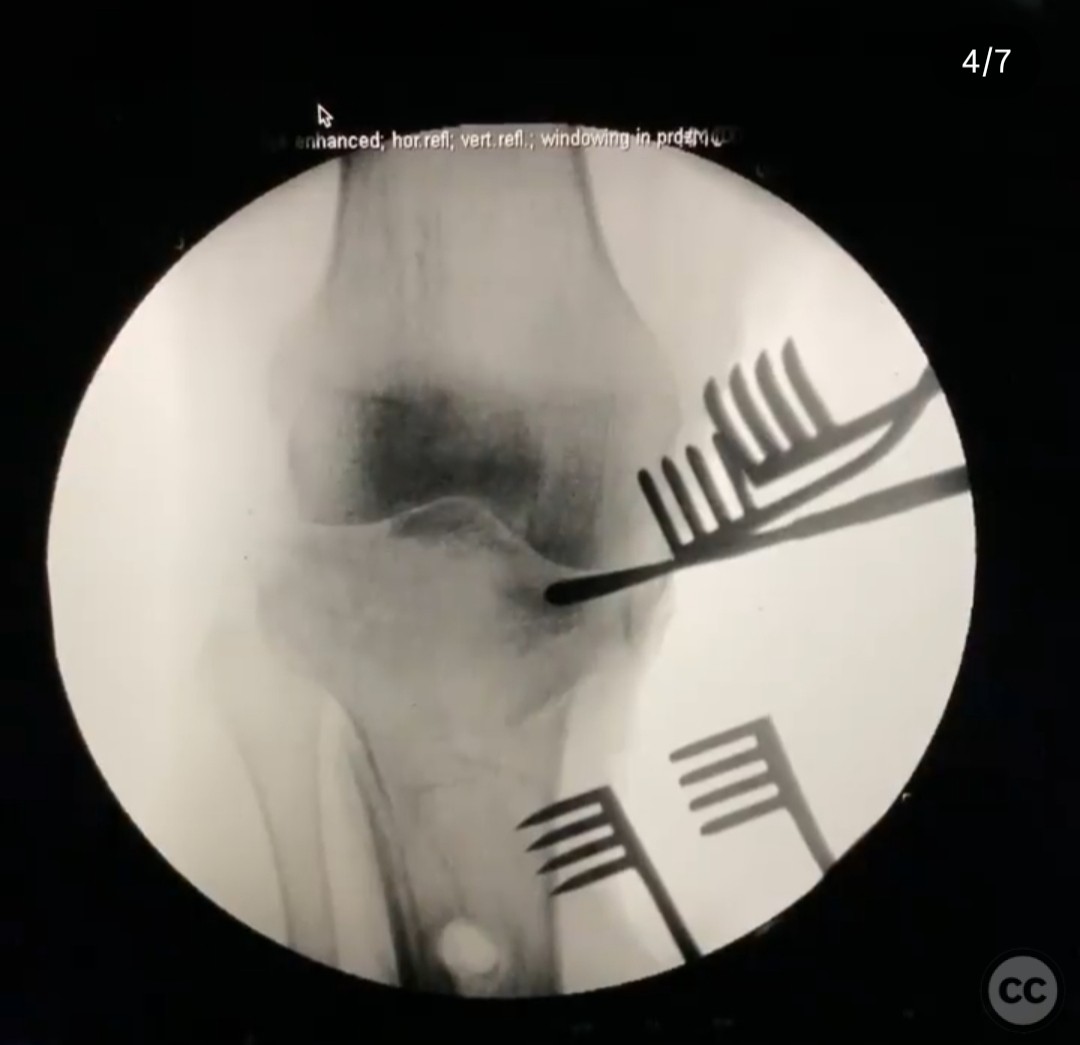
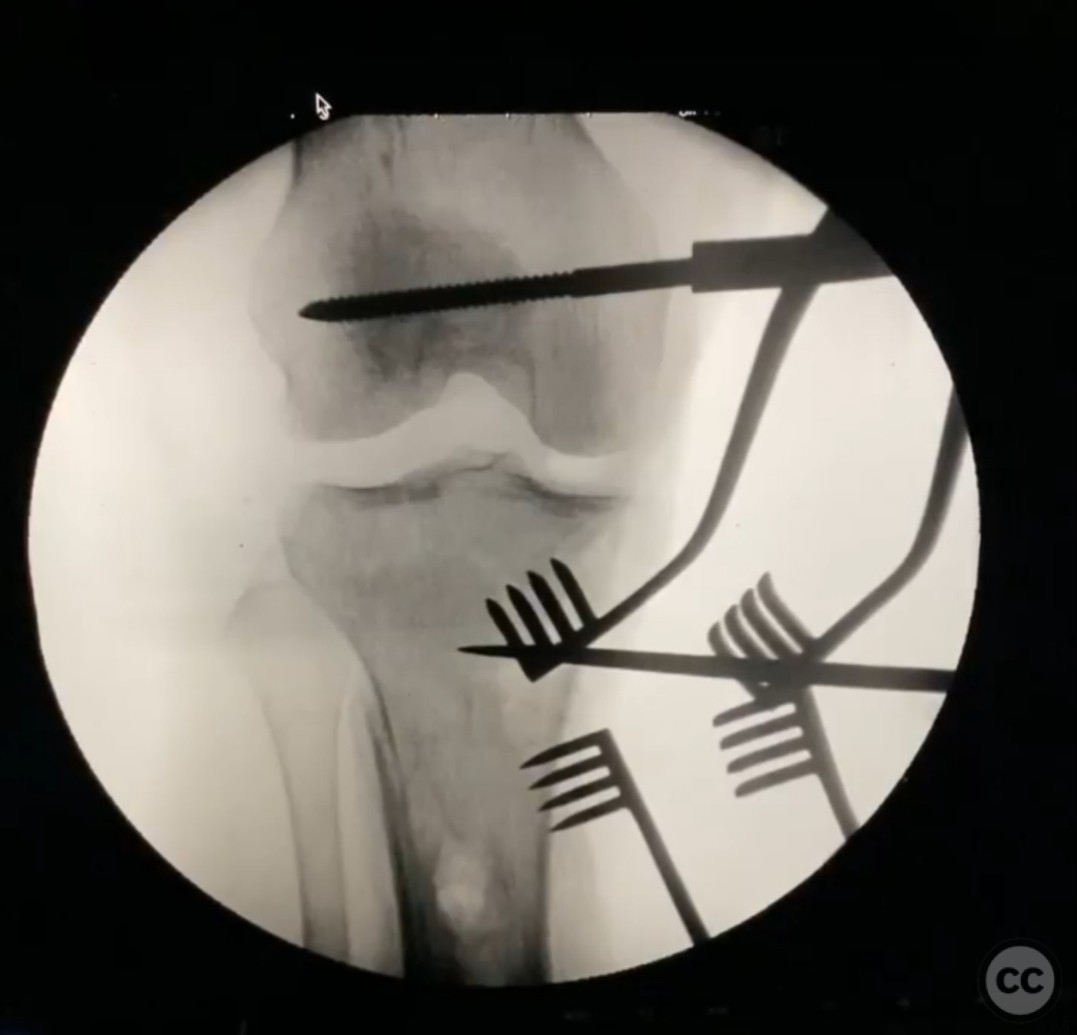
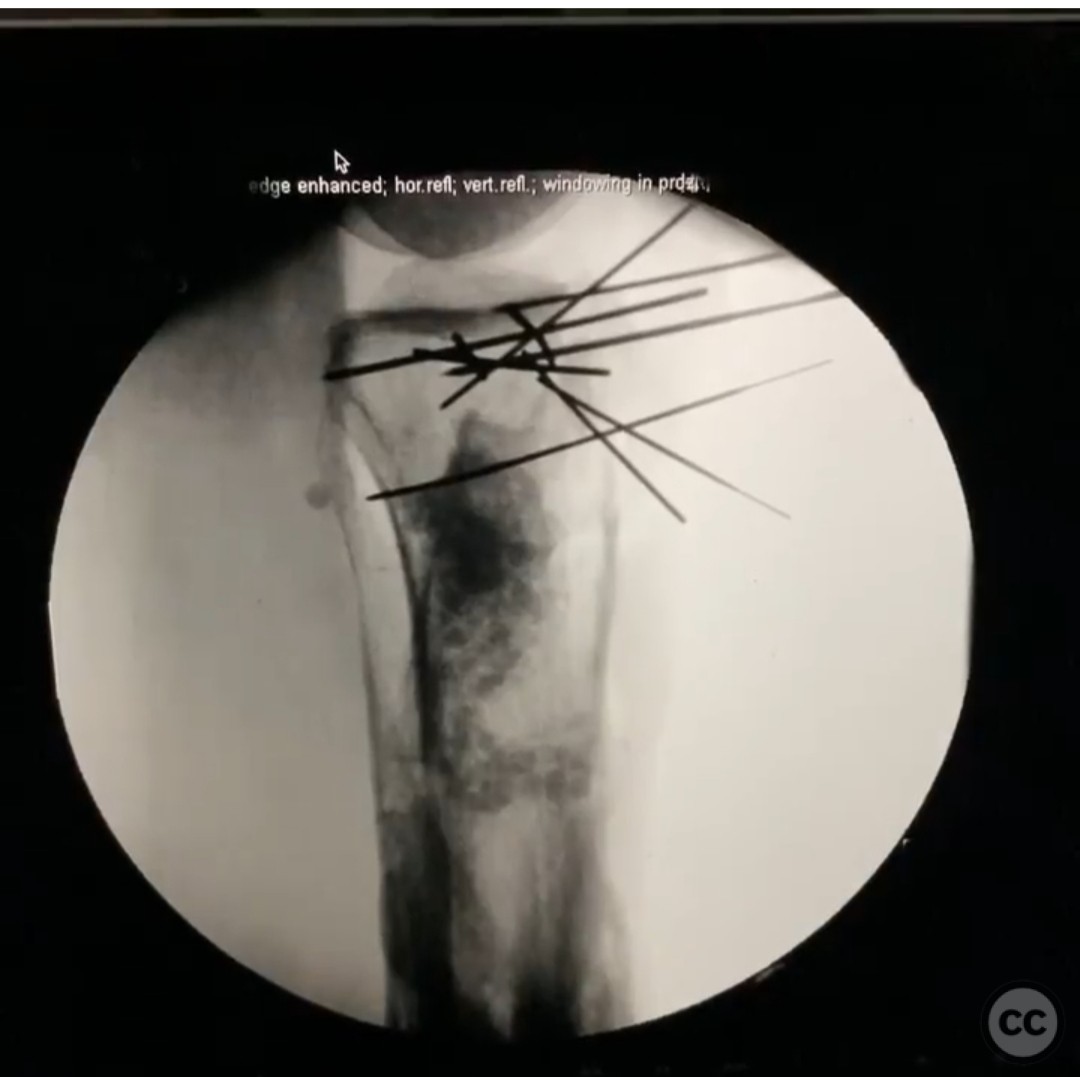
Clinical and radiological findings: A 47-year-old female with type 1 diabetes and dense peripheral neuropathy presented with a hyperextension varus bicondylar tibial plateau fracture following a fall. The patient had a history of a previous 3a open trimalleolar fracture treated at an outside facility, which resulted in redislocation, infection, and subsequent septic ankle. Initial radiographs and CT imaging confirmed the presence of an anterolateral and anteromedial crush injury with medial joint fragmentation and posterior high tension failure. Laboratory findings showed elevated ESR and CRP levels, suggestive of focal pin site osteomyelitis, although the patient was afebrile with a WBC count of 8.
Preoperative Plan
Planning remarks: The preoperative plan involved aggressive debridement of the infected pin site, irrigation, and fixation of the tibial plateau fracture. The surgical approach included the use of antibiotic-loaded PMMA beads for local infection control and structural support of the articular fragments. An anteromedial and direct medial plating strategy was planned to provide buttress support and prevent collapse, followed by lateral side stabilization.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table with a tourniquet applied to the proximal thigh. A medial distractor was utilized to aid in joint reduction.
Anatomical surgical approach: A dual incision approach was employed. The anteromedial incision allowed access to the medial tibial plateau for debridement and plating. A direct medial approach facilitated placement of a buttress plate. The lateral side was accessed through a separate incision for additional stabilization. The articular surface was supported using a PMMA block loaded with antibiotics.
Operative remarks:Intraoperatively, significant attention was given to the meticulous debridement of the infected pin site and removal of necrotic tissue. The use of antibiotic-loaded PMMA beads provided both local infection control and structural support for the articular fragments. The surgeon emphasized the importance of restoring joint congruity and stability to prevent recurrence of the fracture pattern.
Postoperative protocol: Postoperatively, the patient was placed in a hinged knee brace allowing controlled range of motion exercises. Weight-bearing was restricted for 6 weeks, followed by gradual progression to full weight-bearing as tolerated. Antibiotic therapy was continued based on culture sensitivities.
Follow up: Not specified
Orthopaedic implants used: Antibiotic-loaded PMMA beads, medial buttress plate, lateral stabilization plate
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities
















Article viewed 185 times
15 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Hyperextension Varus Bicondylar Tibial Plateau Fracture in a Diabetic Patient with Peripheral Neuropathy. Journal of Orthopaedic Surgery and Traumatology. Case Report 29707008 Published Online Jul 15 2025.