Displaced Comminuted Associated Both Column Acetabular Fracture with Greater Sciatic Notch Fragment and Ipsilateral Sacroiliac Disruption in a Young Adult
Score and Comment on this Case
Clinical Details
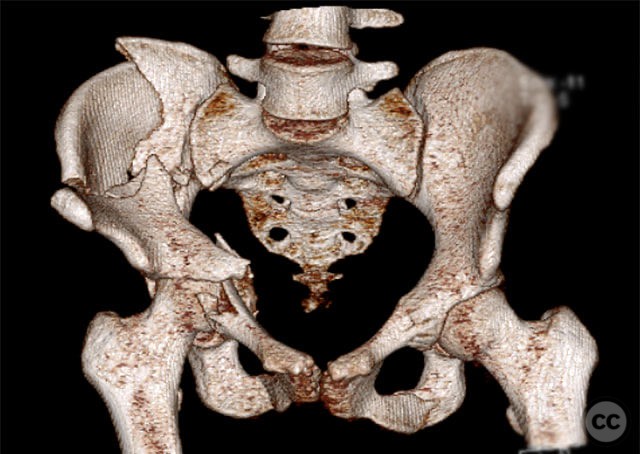
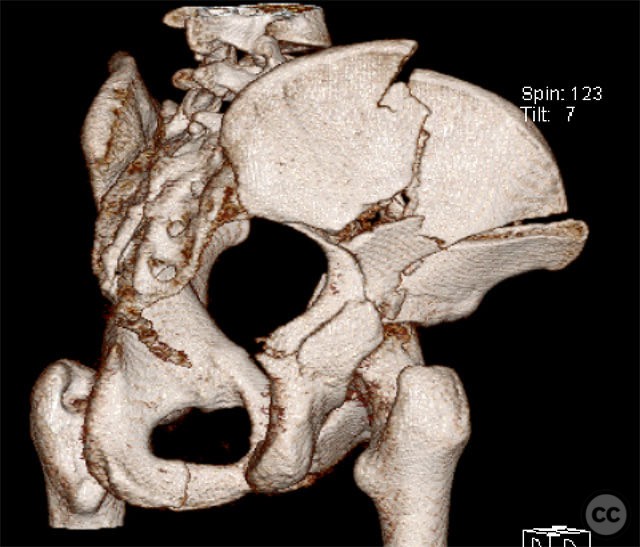
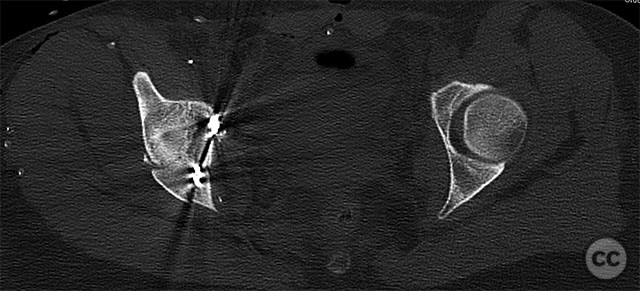
Clinical and radiological findings: A 19-year-old female sustained a high-energy injury in a motor vehicle accident. Initial AP pelvic radiograph demonstrated a right-sided, displaced, comminuted associated both column acetabular fracture (AO/OTA 62C3), with a separate fracture fragment involving the greater sciatic notch (GSN). The right sacroiliac (SI) joint was incompletely disrupted. Surface rendered CT images confirmed the complex fracture morphology, including the separate GSN fragment and the SI-sacral injury, which rendered the typical posterior iliac fragment non-intact. Axial CT at the acetabular dome level revealed multiple displaced fragments and provided further detail regarding soft tissue involvement.
Preoperative Plan
Planning remarks: The preoperative plan involved an ilioinguinal approach (Letournel), utilizing the iliac, vascular, and intrapelvic intervals to access the anterior column, posterior column, GSN fragment, and SI joint. The sequence of reduction was planned as follows: initial reduction and screw fixation of the SI joint injury, followed by reduction of the anterior column fragment, then reduction and clamping of the GSN fragment via the intrapelvic interval, with lag screw fixation through the initial plate, and finally stabilization of the posterior column.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent operating table to facilitate intraoperative fluoroscopy and allow access for an ilioinguinal approach.
Anatomical surgical approach: A standard ilioinguinal approach was performed, with sequential development of the lateral (iliac), middle (vascular), and medial (intrapelvic) windows. Subperiosteal dissection was carried out along the internal iliac fossa to expose the iliac wing and greater sciatic notch. The vascular interval was developed between the external iliac vessels and the iliopsoas muscle. The intrapelvic interval allowed direct access to the quadrilateral surface and GSN fragment. Reduction clamps were applied as required for provisional stabilization.
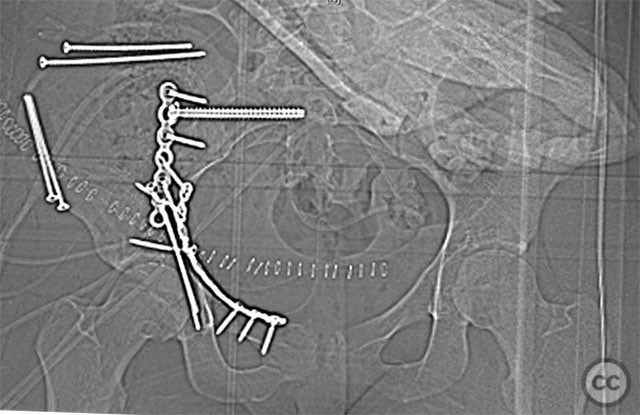
Operative remarks:The SI joint injury was addressed first, with reduction under direct visualization and percutaneous screw fixation across the SI joint. The anterior column fragment was then reduced anatomically. The separate GSN fragment was identified and reduced using clamps via the intrapelvic window; a lag screw was placed through the initial reconstruction plate to secure this fragment. The posterior column was subsequently reduced and stabilized with additional fixation as indicated by intraoperative assessment. The presence of a separate GSN fragment and ipsilateral SI injury necessitated careful sequencing of reduction and stable fixation to restore pelvic ring integrity.
Postoperative protocol: Postoperatively, toe-touch weight bearing was instituted on the affected side for 8 weeks, with progressive increase to partial weight bearing at 8–12 weeks, advancing to full weight bearing by 12–16 weeks as radiographic healing permitted. Early passive and active-assisted range of motion exercises for the hip were initiated from postoperative day one.
Follow up: Not specified
Orthopaedic implants used: Pelvic reconstruction plate(s), cannulated SI screw(s), lag screw(s)
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities



Article viewed 141 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Displaced Comminuted Associated Both Column Acetabular Fracture with Greater Sciatic Notch Fragment and Ipsilateral Sacroiliac Disruption in a Young Adult. Journal of Orthopaedic Surgery and Traumatology. Case Report 29561720 Published Online Sep 11 2025.