Percutaneous Stabilization of Unstable Minimally Displaced Pelvic Ring Injury
Score and Comment on this Case
Clinical Details
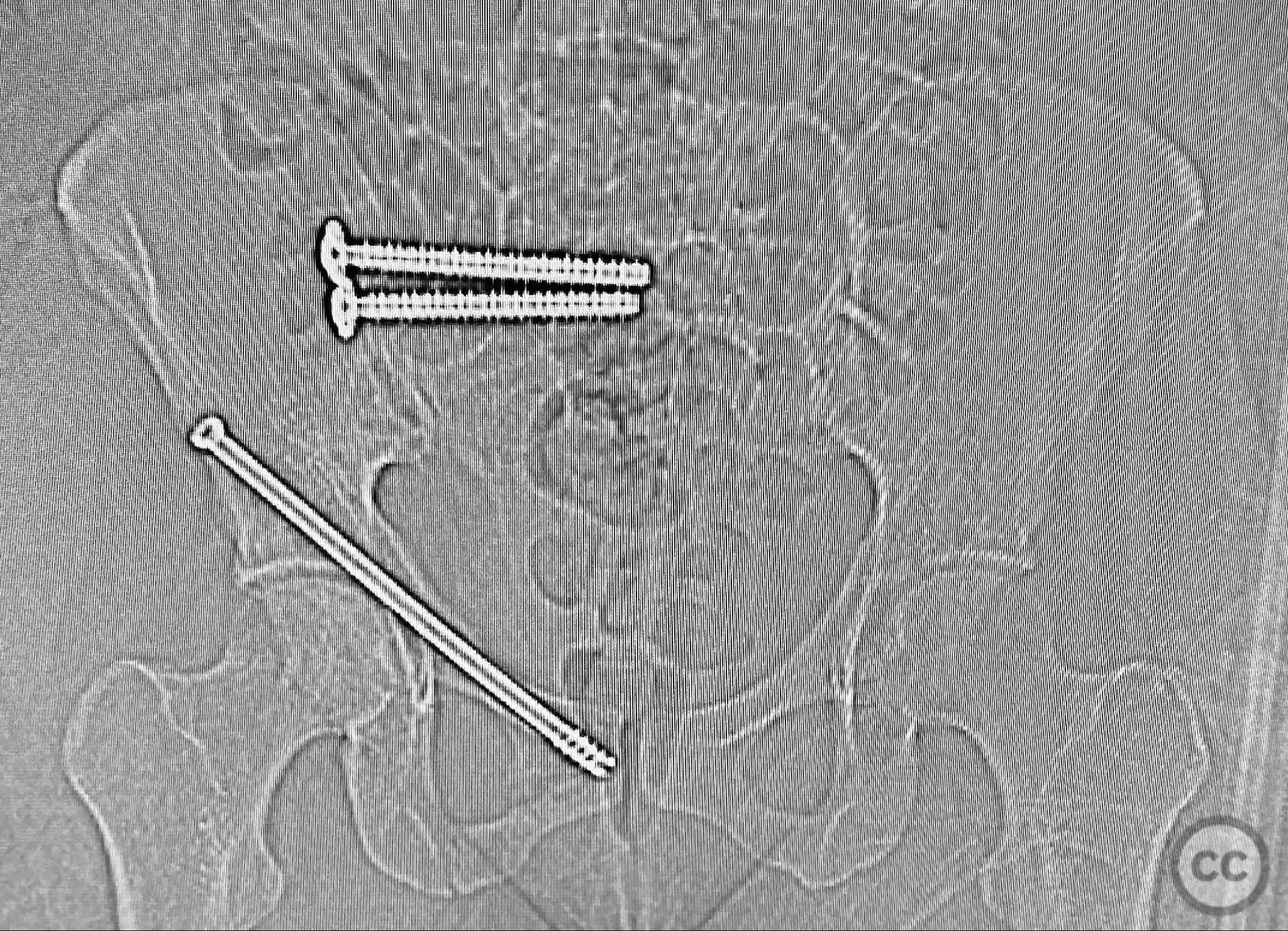
Clinical and radiological findings: A middle-aged patient involved in a motor vehicle collision presented initially with a closed ankle fracture-dislocation and minimal pelvic complaints. Following closed reduction and splinting of the ankle, the patient developed severe pelvic pain (9/10) with any attempted movement. Neurological and vascular examination was not specified. Computed tomography demonstrated minimally displaced fractures of the posterior ilium, sacral ala, and bilateral pubic rami. AP CT surface renderings revealed subtle but clinically significant displacement and deformity of the pelvic ring, which was difficult to appreciate on standard axial images.
Preoperative Plan
Planning remarks: The preoperative plan was to assess pelvic stability under anesthesia, utilizing manual compression of the cristae iliacae with intraoperative fluoroscopic inlet imaging to identify sites of instability. Percutaneous screw fixation was planned for unstable zones, with reduction refined as necessary under imaging guidance.
Surgical Discussion
Patient positioning: Supine position on a radiolucent table, allowing unobstructed fluoroscopic access to the pelvis in multiple planes.
Anatomical surgical approach: Percutaneous approach: Small stab incisions were made over the crista iliaca and sacral entry points as determined by preoperative imaging. Under fluoroscopic guidance, guidewires were advanced across the sacroiliac joint and sacral ala as indicated. Cannulated screws were inserted percutaneously to stabilize the unstable posterior pelvic ring and rami fractures.
Operative remarks:Intraoperative assessment confirmed instability at the posterior pelvic ring with manual stress testing under fluoroscopy. Reduction was achieved with gentle manipulation and maintained during percutaneous screw insertion. The use of intraoperative inlet and outlet views was critical for accurate screw placement and confirmation of reduction. The minimally invasive technique minimized additional soft tissue trauma in this polytrauma patient.
Postoperative protocol: Early mobilization as tolerated with protected weight bearing for 6–8 weeks. Progressive increase in activity based on radiographic evidence of healing and clinical improvement in pain. Emphasis on deep vein thrombosis prophylaxis and pulmonary hygiene.
Follow up: Not specified
Orthopaedic implants used: Cannulated percutaneous pelvic screws
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities








Article viewed 134 times
12 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Percutaneous Stabilization of Unstable Minimally Displaced Pelvic Ring Injury. Journal of Orthopaedic Surgery and Traumatology. Case Report 28127312 Published Online Sep 12 2025.