Proximal tibiofibular dislocation
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: coming
Preoperative Plan
Planning remarks: coming
Surgical Discussion
Patient positioning: Supin with a 45deg bump
Anatomical surgical approach: Direct lateral
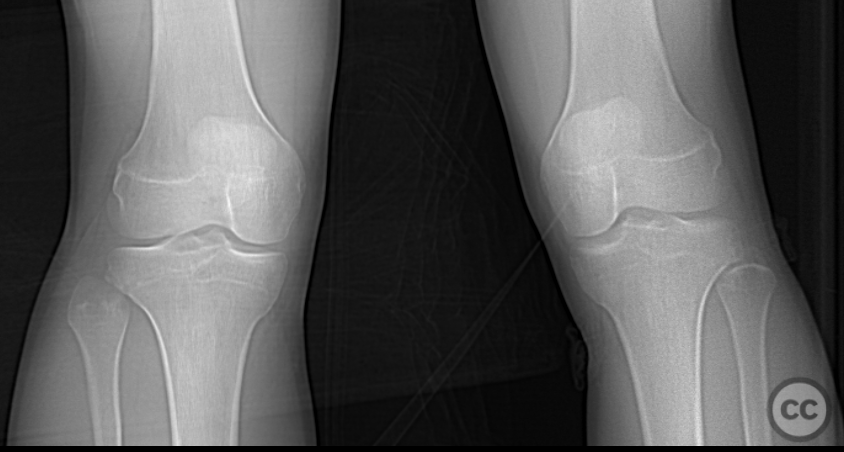
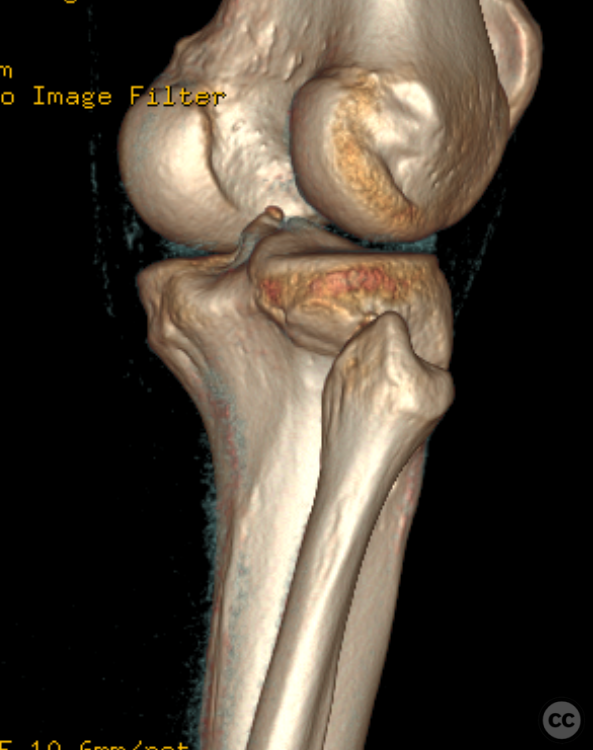
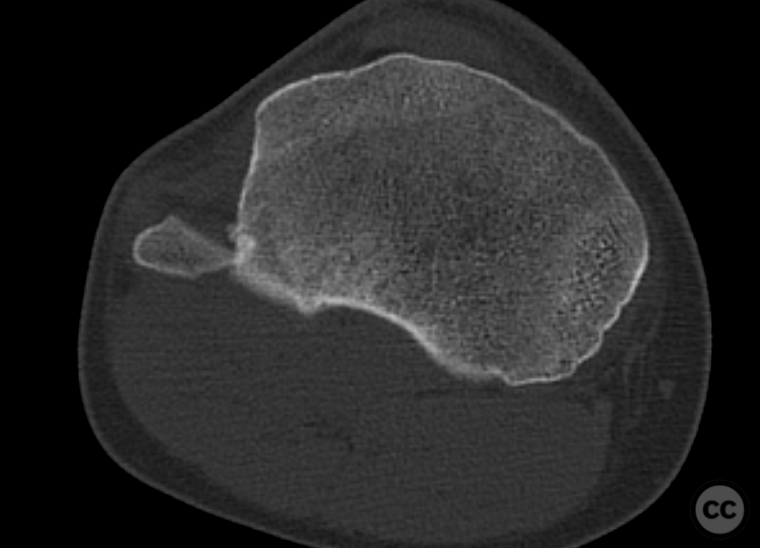
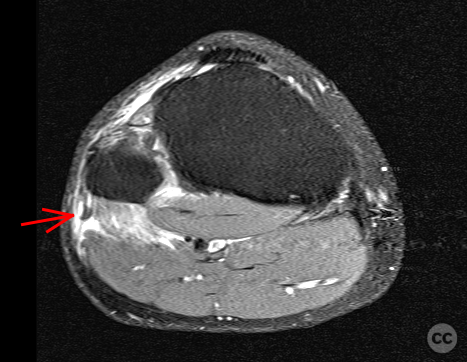
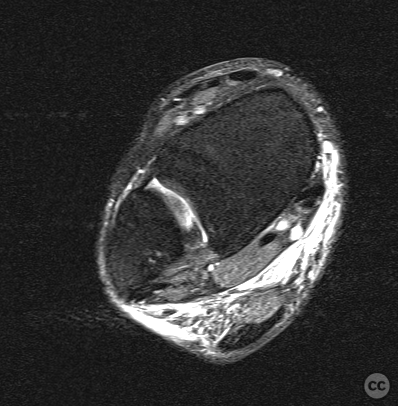
Operative remarks:The patient was positioned supine on a radiolucent operating table, with the right leg elevated on a 45-degree pillow. A tourniquet was applied to the ipsilateral thigh, followed by a sterile preparation and draping of the operative field. A timeout was conducted, and two grams of cefazolin antibiotics were administered. Preoperative computed tomography (CT), magnetic resonance imaging (MRI), and plain film imaging revealed a perched anterior dislocation of the proximal tibiofibular joint. Notably, the common peroneal nerve was not entrapped, and there was no identifiable injury to the structures of the posterolateral corner, including the popliteus complex and the lateral collateral ligament. Local soft tissue examination indicated a rupture of the capsule and stabilizing ligaments of the proximal tibiofibular joint. A longitudinal incision was made over the palpable fibular head, measuring approximately seven centimeters in length, followed by subcutaneous dissection and splitting of the fascia. Exploration of the biceps muscle allowed for identification of the course of the peroneal nerve along its posterior margin. Dissection continued to the level of the fibular head, where neurolysis and mobilization of the nerve around the neck of the fibula were performed, ensuring no iatrogenic injury to the nerve during repositioning. Attempts to reduce the perched dislocation through manual manipulation were unsuccessful. Consequently, a secondary soft tissue window was created anterior to the tibiofibular joint, and the introduction of a blunt periosteal elevator facilitated the application of leverage, resulting in a satisfactory spontaneous relocation of the joint to its anatomic position. Live fluoroscopy demonstrated significant diastasis and instability of the joint despite anatomic reduction. Therefore, the decision was made to perform TightRope stabilization, ensuring protection of the nerve and utilizing multi-plane arthroscopy. The introduction of a 3.7-millimeter cannulated drill was executed in a quadricortical manner from a posterolateral to anteromedial direction, followed by the insertion of an Arthrex fibula syndesmosis TightRope, which was tensioned on the lateral side. Subsequent dynamic fluoroscopy confirmed anatomic reduction and stability. Joint irrigation was performed, followed by reinspection of the nerve, which exhibited no iatrogenic injuries. The procedure concluded with closure of the fascia, subcutaneous tissue, and running sutures for the skin. Sterile dressings and an elastic bandage were applied. No postoperative orthosis was deemed necessary.
Postoperative protocol: FWB. No port 3Months
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisManagement of proximal tibiofibular dislocation primarily involves prompt diagnosis and appropriate intervention, with surgical stabilization being favored in cases of chronic instability or associated vascular injuries. Conservative management is suitable for acute, isolated dislocations without significant instability or complications. Early recognition and tailored treatment strategies are essential to prevent chronic instability and optimize functional outcomes.
Evidence and Analysis:
Kruckeberg et al. [1] conducted a systematic review evaluating treatment options for proximal tibiofibular joint (PTFJ) instability. Out of 44 studies encompassing 96 patients, 35 were managed nonoperatively. The review highlighted that surgical interventions, particularly proximal tibiofibular ligament reconstructions, led to improved outcomes with lower complication rates compared to nonoperative methods. However, PTFJ fixation was associated with a 28% complication rate, and fibular head resection had a 20% complication rate, underscoring the risks inherent in surgical management.
Rajan et al. [2] presented a systematic review alongside a retrospective analysis of 17 patients with traumatic PTFJ dislocations treated at a level 1 trauma center. The study revealed that 94.1% of these dislocations were associated with fractures, predominantly tibial shaft fractures (68.75%). Vascular injuries were present in 29.4% of cases, necessitating surgical intervention. Alarmingly, 47% of patients underwent amputation, with higher rates observed in those with open fractures (87.5%) and vascular injuries (50%). This study emphasizes the severity of PTFJ dislocations when accompanied by other injuries and suggests that surgical management is often required to address complex trauma, though it carries significant risks.
Sarma et al. [3] provided a comprehensive review of PTFJ anatomy, biomechanics, and traumatic pathology. They emphasized the necessity of early diagnosis to prevent chronic instability and extensive surgical interventions. The review suggested that nonoperative treatment might lead to persistent symptoms, whereas surgical stabilization can restore normal joint biomechanics and improve functional outcomes, especially in athletic populations. However, the reliance on Level IV evidence limits the strength of these conclusions.
Curatolo et al. [4] reviewed common clinical conditions affecting the PTFJ, including dislocations and chronic instability. Their analysis advocated for a multidisciplinary approach in managing PTFJ injuries, highlighting that early surgical intervention results in better outcomes. The review discussed diagnostic challenges and proposed that conservative management may be insufficient in cases with structural ligament damage, aligning with the findings of higher complication rates in surgical interventions noted by Kruckeberg et al.
Yuan et al. [5] examined the diagnosis and treatment of PTFJ dislocations within a Chinese cohort. They reported that PTFJ dislocations are often associated with tibial and fibular fractures, complicating diagnosis due to atypical radiographic presentations. The study recommended routine use of advanced imaging modalities, such as CT scans, to ensure accurate diagnosis and appropriate management. They underscored the importance of open reduction in restoring joint stability, particularly in Maisonneuve fractures, thereby supporting the surgical interventions advocated by other studies.
Rozhl Chir [6] (2020) and [7] (2023) focused on Maisonneuve fractures, a specific type of PTFJ injury. The 2020 study by Kašper et al. included 70 patients, noting that 76.5% had open fractures and 29.4% had vascular injuries requiring surgical intervention. The 2023 study further emphasized the complexity of Maisonneuve fractures, advocating for anatomical reduction of the distal fibula and the use of postoperative CT scans to verify alignment. Both studies highlighted the critical nature of surgical management in complex PTFJ injuries to prevent chronic deficits and ensure joint stability.
Cunningham et al. [8] addressed isolated PTFJ dislocations in an emergency medicine context. They noted that while isolated PTFJ dislocations are rare and often manageable with nonoperative approaches, the lack of consensus on definitive management highlights the necessity for individualized treatment plans based on injury severity and associated complications. Their practical management approach aligns with the need for prompt diagnosis and tailored interventions discussed in other studies.
Overall, the evidence suggests a dichotomy in managing PTFJ dislocations: conservative management may be appropriate for acute, isolated cases without significant instability or vascular injury, while surgical intervention is often necessary in chronic instability or cases with associated fractures and vascular damage. The high complication rates associated with surgical treatments, as reported by Kruckeberg et al. and Rajan et al., indicate the need for careful patient selection and operative planning. However, the predominance of Level IV evidence among the studies limits the robustness of these conclusions, highlighting the need for higher-level research to establish standardized management protocols.
Discussion:
The management of proximal tibiofibular dislocation is nuanced, contingent upon the acuity of the injury and the presence of associated complications. Acute, isolated PTFJ dislocations without significant ligamentous damage or vascular compromise can often be managed conservatively with immobilization and physical therapy. However, the literature reviewed underscores that cases involving chronic instability, concomitant fractures, or vascular injuries necessitate surgical intervention to restore joint integrity and prevent adverse outcomes such as chronic instability or limb loss.
Surgical options, while effective in stabilizing the joint, carry inherent risks, including infection and nerve injury, as demonstrated by the high complication rates reported in systematic reviews. Therefore, the decision to proceed with surgery must weigh the benefits of joint stabilization against the potential for surgical complications. Moreover, the high incidence of associated injuries, particularly in traumatic PTFJ dislocations, requires a comprehensive diagnostic approach, including advanced imaging, to ensure accurate assessment and appropriate management.
The current state of evidence, predominantly consisting of Level IV studies, indicates a lack of high-quality, randomized controlled trials to definitively guide the management of PTFJ dislocations. Consequently, clinical practice relies on retrospective analyses and expert consensus, which may not fully capture the nuances of patient variability and injury complexity. Future research should aim to establish higher-level evidence to inform standardized treatment protocols for proximal tibiofibular dislocations, improve diagnostic accuracy, and optimize functional outcomes for patients.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities












Article viewed 656 times
22 Aug 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Proximal tibiofibular dislocation. Journal of Orthopaedic Surgery and Traumatology. Case Report 27249978 Published Online Aug 22 2024.