Open Tibia IIIC Fracture with Soft Tissue Defect and Infection Management
Score and Comment on this Case
Clinical Details
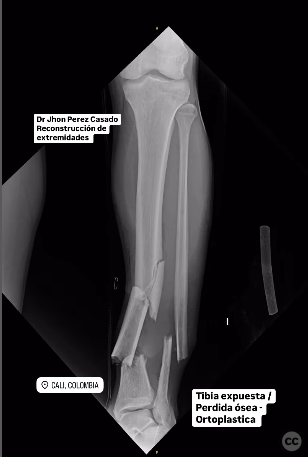
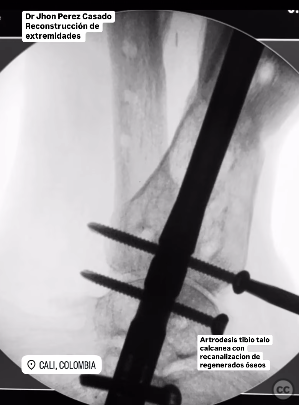
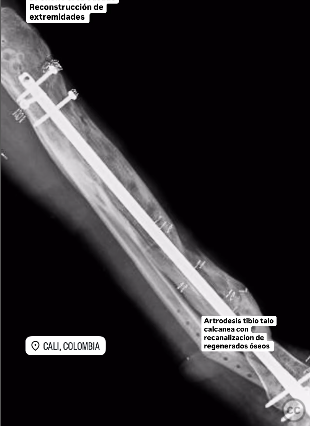
Clinical and radiological findings: A young adult presented with an open tibial fracture classified as Gustilo-Anderson Type IIIC, indicating a high-energy injury with extensive soft tissue damage and vascular compromise. Initial clinical examination revealed exposed bone tissue with contamination. Radiological assessment confirmed the fracture of the tibia with significant bone loss and soft tissue defect.
Preoperative Plan
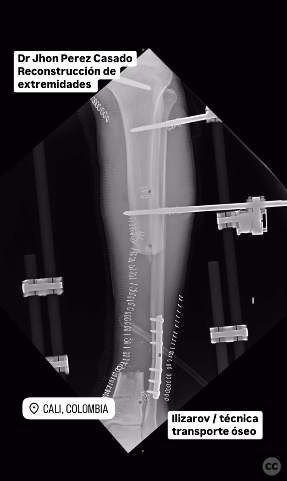
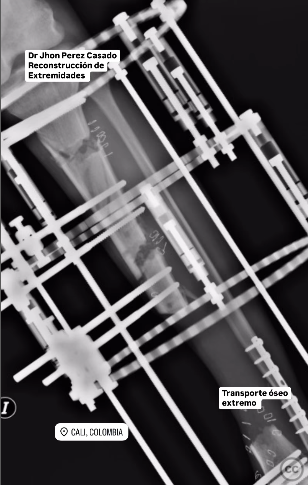
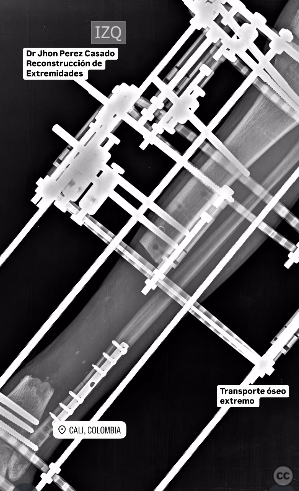
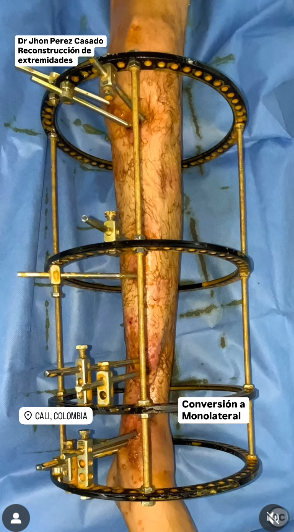
Planning remarks: The preoperative plan involved radical debridement of contaminated and necrotic tissue, followed by direct wound closure. An Ilizarov external fixator was initially applied for bifocal bone transport at a rate of 1 mm per day to address the bone defect. Conversion to a monolateral external fixator was planned to facilitate subsequent soft tissue coverage procedures.
Surgical Discussion
Patient positioning: The patient was positioned supine for ease of access to both the anterior and posterior aspects of the lower leg, allowing for comprehensive debridement and fixation.
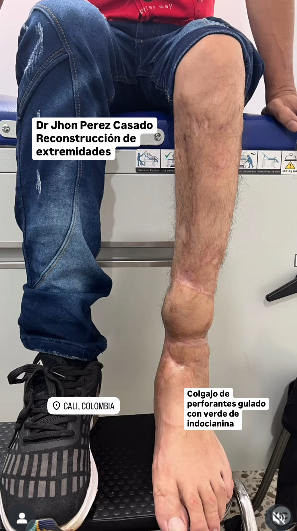
Anatomical surgical approach: The surgical approach involved a meticulous radical debridement of all necrotic and contaminated tissues, followed by direct closure of the wound. The Ilizarov frame was applied circumferentially around the tibia for stabilization and bone transport. A reverse sural flap based on the peroneal artery perforator was planned for coverage of the soft tissue defect at the docking site.
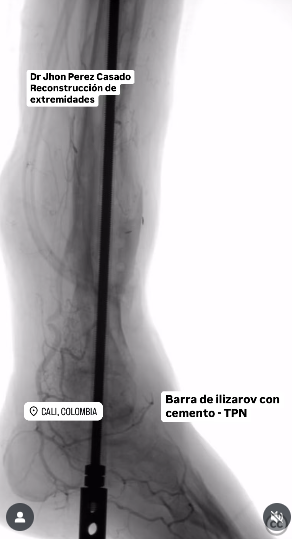
Operative remarks:During the procedure, a two-stage modified sural perforator flap was executed, with initial flap elevation and delayed inset to ensure optimal perfusion. Temporary negative pressure wound therapy (TPN) was utilized to prevent screw extraction complications. The application of morphogenetic protein at the bone docking site was performed to enhance osteogenesis. Subsequent reactivation of infection required removal of hardware and medullary canal debridement using RIA2, followed by insertion of an antibiotic-releasing nail.
Postoperative protocol: Postoperative rehabilitation included non-weight bearing on the affected limb until adequate soft tissue healing and bone consolidation were achieved. Gradual weight-bearing was introduced as tolerated, with close monitoring for signs of infection or flap compromise.
Follow up: Not specified.
Orthopaedic implants used: Ilizarov external fixator, monolateral external fixator, reverse sural flap, TPN system, RIA2 system, antibiotic-releasing intramedullary nail.
Search for Related Literature

Jhon Perez Casado
- Colombia , Cali - Valle del Cauca
- Area of Specialty - Lower Limb
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities







Article viewed 192 times
23 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Perez Casado, J.J.. (2025). Open Tibia IIIC Fracture with Soft Tissue Defect and Infection Management. Journal of Orthopaedic Surgery and Traumatology. Case Report 24677200 Published Online Jul 23 2025.