Geriatric 'Snowboarder' fracture - Lateral talar process + fibula fracture
Score and Comment on this Case
Clinical Details
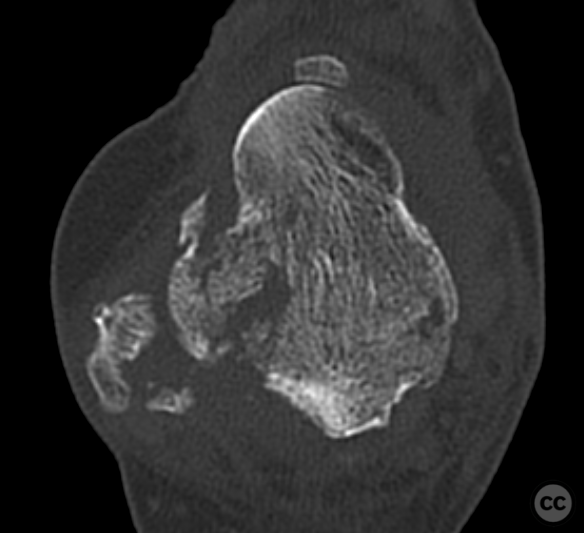
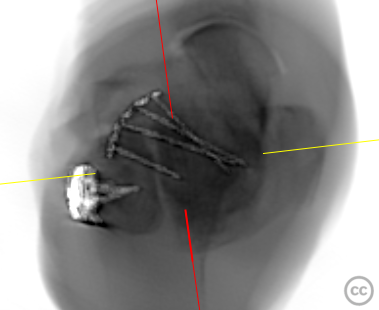
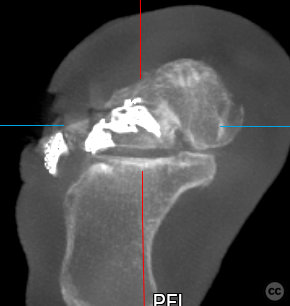
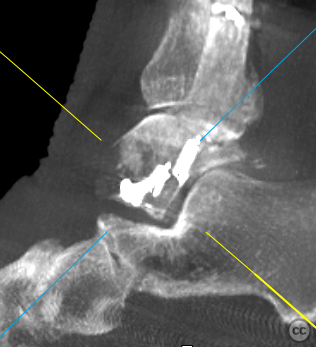
Clinical and radiological findings: A unique injury of a dorsiflexed 'brake foot' injury sustained by an 85yo F in a motor vehicle accident. Whilst the classical 'snowboarder' fracture is seen in the dorsiflexed foot under high axial load and external rotation, a similar load constellation may be experienced by a dorsiflexed foot on a brake pedal under heavy breaking prior to frontal collision where a peak axial impulse force occurs.
Preoperative Plan
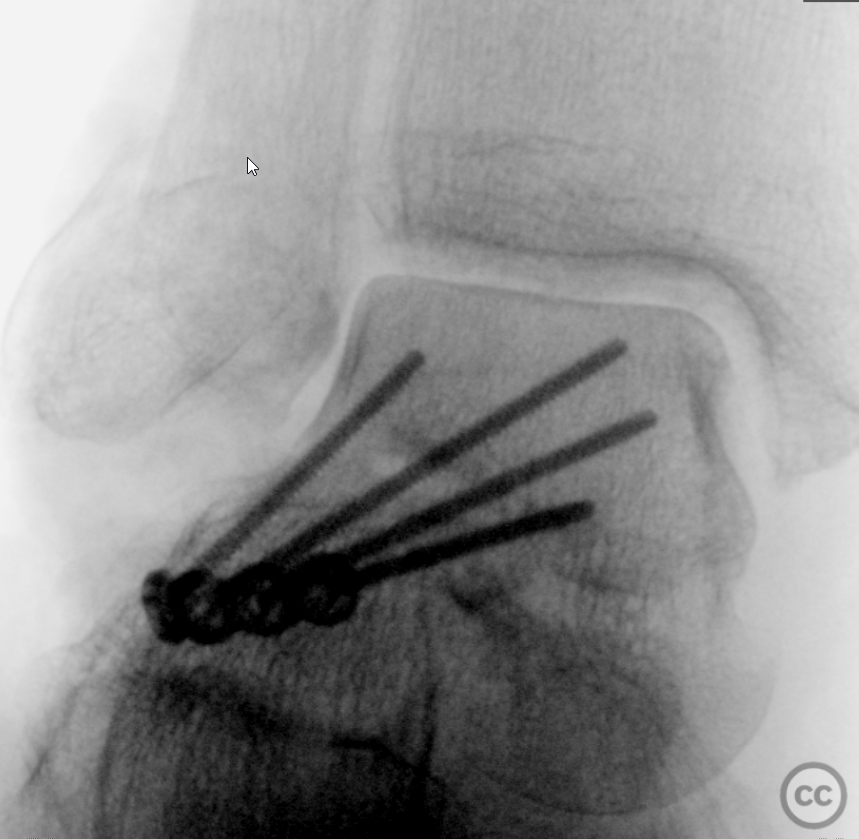
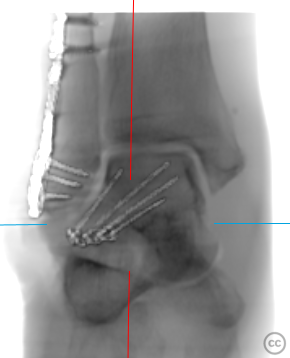
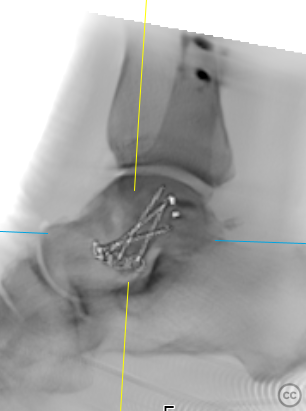
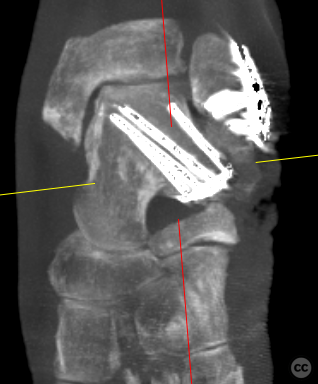
Planning remarks: Initial consideration was given to simple cannulated screw fixation, however given the osteoporotic nature of the bone and the low pull-out strength of individual screws , this was considered insufficient. Instead we chose to anchor the LTP with a small 2.0mm locking plate, utilising divergent locked screws in the plate to prevent failure of fixation and loss of reduction under load.
Surgical Discussion
Patient positioning: Supine
Anatomical surgical approach: Single curved incision over the distal fibula curving anteriorly over the LTP and extending distally in line with the 4th MT Ray
Operative remarks:coming
Postoperative protocol: NWB/TWB 8W in an ankle Orthosis. ROM exercise out of the Orthosis allowed
Orthopaedic implants used: Stryker 2.0mm Minifragment plate (Talus) Synthes 3.5/2.7mm LCP distal locking fibula plate
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisArticles:
A total of 11 articles were analyzed in the generation of this review. The collection includes systematic reviews, retrospective and prospective case series, clinical reviews, case reports, and expert narrative reviews. The evidence levels range predominantly from Level IV (case series and retrospective studies) to Level V (expert opinion and narrative reviews), with no randomized controlled trials or large prospective cohort studies identified. The publication dates span from 1994 to 2023, reflecting over two decades of evolving understanding of snowboarder’s talus fractures.
TLDR:
Snowboarder’s talus fractures predominantly involve the lateral process of the talus (LPTF), a rare but clinically significant injury often misdiagnosed as a severe ankle sprain. These fractures result from a mechanism of dorsiflexion and inversion of the ankle, frequently associated with soft-shell snowboarding boots and aerial maneuvers. Early diagnosis using advanced imaging (CT and MRI) is critical due to the high rate of missed injuries on plain radiographs. Treatment is dictated by fracture displacement and comminution: nondisplaced fractures can be managed conservatively with immobilization and protected weight-bearing, while displaced or comminuted fractures require surgical fixation to prevent long-term morbidity including subtalar arthritis and chronic pain. Long-term outcomes are generally favorable when treatment is timely and appropriate, but the evidence base remains limited to retrospective case series and expert opinion, necessitating further prospective studies.
Evidence and Analysis:
The literature consistently identifies the lateral process of the talus as the anatomical site most commonly implicated in snowboarder’s talus fractures, often termed “snowboarder’s ankle” [10,8,3]. Nicholas et al. (1994) first characterized this injury, highlighting its frequent misdiagnosis due to clinical similarity to lateral ankle sprains and subtle radiographic findings [10]. McCrory and Bladin (1996) further elaborated on the injury mechanism, attributing it to combined dorsiflexion and inversion forces, with soft-shell boots and aerial maneuvers increasing risk [8]. This pathomechanics aligns with the anatomical description provided by Russell and Byerly (2023), emphasizing the lateral process’s articulation with the fibula and subtalar joint, and its vulnerability during forced inversion [2].
Epidemiological data from Bladin and McCrory (1995) and Young and Niedfeldt (1999) underscore the injury’s rarity but increasing incidence paralleling snowboarding’s popularity [5,4]. Bladin et al. reported an injury rate of 4-6 per 1000 visits with ankle injuries comprising 23% of lower limb injuries, and lateral process fractures constituting a small subset often overlooked [5]. Young and Niedfeldt emphasized the need for high clinical suspicion in “severe ankle sprains” unresponsive to treatment [4].
Diagnostic challenges are well documented. Kramer et al. (2014) presented a case report and literature review emphasizing the frequent initial oversight of LPTF on plain radiographs due to subtle fracture lines and overlapping anatomy [3]. Hörterer et al. (2018) analyzed eight retrospective studies (each with ≥7 patients) and concluded that plain radiographs are insufficient, recommending CT and MRI to assess fracture morphology and concomitant soft tissue injuries such as peroneal tendon dislocation (46%) and chondral lesions (48%) [7]. This is supported by Wijers et al. (2020), who analyzed 36 patients with LPTF treated at a Level 1 trauma center and underscored the role of advanced imaging in classification and surgical planning [11].
Classification systems for LPTF have evolved but remain imperfect. The McCrory-Bladin classification, dividing fractures into three types based on severity, remains widely used but has been criticized for insufficient granularity [6,8]. Tinner and Sommer (2018) proposed a refined classification subdividing multifragmented type III fractures into three subtypes (IIIa, IIIb, IIIc) to better guide treatment decisions [6]. Wijers et al. (2020) further proposed a modified classification incorporating fracture severity and intra- versus extra-articular involvement, demonstrating its utility in prognostication and management [11].
Treatment paradigms hinge on fracture displacement and comminution. Conservative management, typically immobilization and partial weight-bearing for six weeks, is reserved for nondisplaced or minimally displaced fractures [7,6,11]. Hörterer et al. (2018) recommend surgical fixation for dislocated fractures (>2 mm displacement), citing better functional outcomes and reduced risk of subtalar arthritis [7]. Wijers et al. reported that 78% of their 36 patients underwent operative fixation, with a median American Orthopaedic Foot and Ankle Society (AOFAS) Hindfoot Score of 75 (range 12-100) at a mean follow-up of 5.5 years, indicating generally good long-term function [11]. However, variability in outcomes and some poor scores reflect the heterogeneity of injury severity and treatment timing.
Surgical techniques emphasize anatomic reduction and stable fixation using minifragment plates and screws, often via dual incisions to minimize soft tissue disruption [9]. Shakked and Tejwani (2013) highlight the importance of prompt reduction of dislocations and early operative intervention to mitigate complications such as osteonecrosis, malunion, and post-traumatic arthritis [9]. The lateral process’s tenuous blood supply, predominantly extraosseous and easily disrupted, contributes to the risk of avascular necrosis in displaced fractures [2].
Complications remain a significant concern. Hörterer et al. (2018) noted frequent concomitant injuries including peroneal tendon dislocation and subtalar joint subluxation, which may complicate treatment and outcomes [7]. Delayed or missed diagnosis leads to symptomatic malunion, chronic pain, and subtalar arthritis, as documented in case reports and small series [1,3,11]. Ibrahim et al. (2015) underscore the paucity of high-quality evidence and call for robust prospective studies to validate treatment algorithms [1].
The quality of evidence across all studies is limited by small sample sizes, retrospective designs, and heterogeneity in diagnostic and treatment protocols. No randomized controlled trials or large prospective cohorts exist, and many recommendations derive from expert opinion and case series (Level IV-V evidence). This constrains definitive conclusions but does not diminish the clinical importance of recognizing and appropriately managing snowboarder’s talus fractures.
Discussion:
The snowboarder’s talus fracture, predominantly involving the lateral process, represents a distinct injury pattern characterized by a specific mechanism of dorsiflexion and inversion in the context of snowboarding biomechanics. Despite its rarity, it demands heightened clinical vigilance due to frequent misdiagnosis as an ankle sprain and the significant morbidity associated with delayed or inadequate treatment. The reviewed literature converges on several critical points: the necessity of advanced imaging for accurate diagnosis, the importance of fracture classification to guide treatment, and the preferential surgical management of displaced or comminuted fractures to optimize long-term outcomes.
Conservative treatment remains appropriate for nondisplaced fractures, with immobilization and protected weight-bearing yielding generally favorable results. However, the threshold for surgical intervention must be low in displaced fractures (>2 mm) or those with intra-articular involvement, given the risk of osteonecrosis, malunion, and subtalar arthritis. Surgical techniques should aim for anatomic reduction and stable fixation, with awareness of concomitant soft tissue injuries that may influence prognosis.
The current evidence base, while informative, is limited by retrospective designs and small cohorts, underscoring the urgent need for prospective studies with standardized diagnostic and treatment protocols. Such research would clarify optimal management strategies and improve functional outcomes for this challenging injury.
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities

















Article viewed 1513 times
21 Apr 2023
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2023). Geriatric 'Snowboarder' fracture - Lateral talar process + fibula fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 20610898 Published Online Apr 21 2023.