Extensor Indicis Proprius to Extensor Pollicis Longus Tendon Transfer for Ruptured EPL
Score and Comment on this Case
Clinical Details
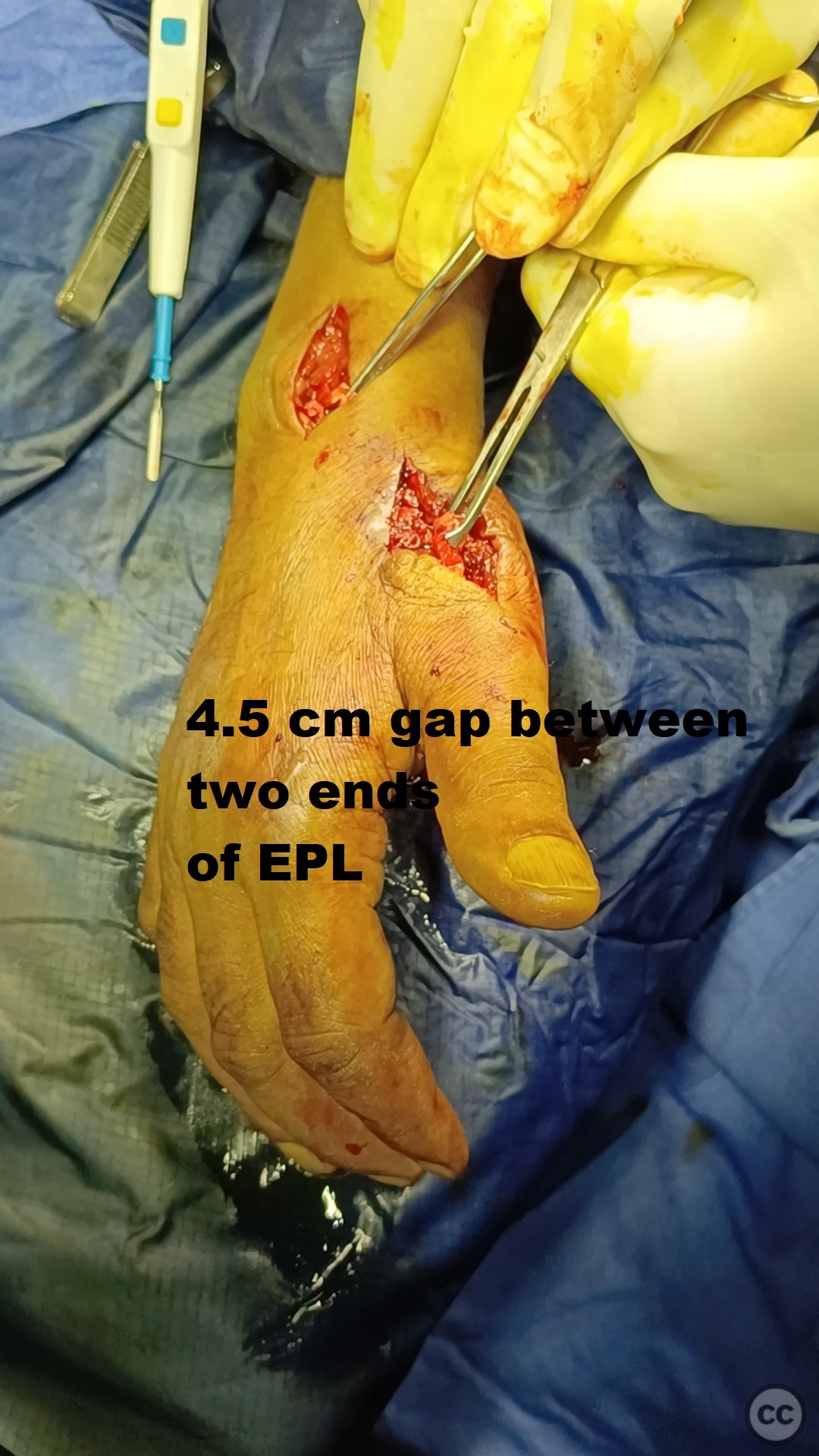
Clinical and radiological findings: A 59-year-old male presented with an inability to extend the interphalangeal joint and MCP joint of the right thumb following cut injury by glass piece. He had undergone initial surgery of alleged tendon repair elsewhere but now at 1 month post op there was no active extension of thumb. Clinical examination revealed a complete loss of active extension at the thumb's interphalangeal joint, consistent with extensor pollicis longus (EPL) tendon rupture. Radiographs of the wrist and hand were unremarkable for fractures or dislocations. An MRI confirmed the rupture of the EPL tendon with distance between two ends of tendon being 4.5 cm.
Preoperative Plan
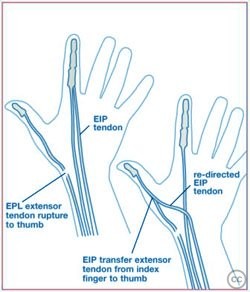
Planning remarks: The preoperative plan involved performing an extensor indicis proprius (EIP) to EPL tendon transfer. The surgical approach was planned via a dorsal incision over the third and fourth extensor compartments to facilitate tendon identification and transfer.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table with the arm placed on an arm board. A pneumatic tourniquet was applied to the upper arm to provide a bloodless field.
Anatomical surgical approach: A longitudinal dorsal incision was made over the distal forearm and wrist, centered over Lister's tubercle. The extensor retinaculum was incised, and the third extensor compartment was opened to identify the ruptured EPL tendon proximal stump. The EIP tendon was identified in the fourth extensor compartment, mobilized, and transferred to the distal stump of the EPL tendon using Pulvertaft weave technique.
Operative remarks:We noted that the EIP tendon had excellent length and tension for transfer, allowing for a robust connection to the EPL stump. Care was taken to ensure that the transferred tendon was tensioned appropriately to restore full thumb extension without causing excessive tightness or limiting flexion.
Postoperative protocol: Postoperatively, the patient was immobilized in a thumb spica splint for four weeks to protect the repair. Gradual mobilization began at four weeks with supervised hand therapy focusing on range of motion and strengthening exercises.
Follow up: nil
Orthopaedic implants used: Proline 3,0 sutures for tendon transfer fixation.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisExtensor indicis proprius (EIP) to EPL tendon transfer is the most widely adopted and effective surgical method for reconstructing extensor pollicis longus (EPL) ruptures, demonstrating favorable functional outcomes, high patient satisfaction, and a low incidence of complications, although alternative techniques are viable when EIP transfer is contraindicated.
Evidence and Analysis:
The reconstruction of the extensor pollicis longus (EPL) tendon following its rupture is critical for restoring thumb functionality. Among the various reconstruction strategies, the transfer of the extensor indicis proprius (EIP) tendon stands out as the most prevalent method. Ganon et al. [1] conducted a systematic review analyzing 18 studies encompassing 515 patients, concluding that EIP transfer remains the preferred modality due to its reliability and minimal postoperative rehabilitation requirements. In their review, follow-up durations averaged 28 months, underscoring the sustained efficacy of EIP transfers over time.
Supporting this, Stirling et al. [6] presented a cohort study involving 12 patients, where EIP transfer significantly improved QuickDASH scores from a mean of 29.7 preoperatively to 15.2 postoperatively (p=0.05), alongside enhancements in health-related quality of life metrics. The study’s Level III evidence provides moderate support for the procedure's effectiveness, although the small sample size warrants cautious interpretation.
Retrospective case series further reinforce these findings. Cha et al. [2] reported five cases where primary EPL repair was feasible in select patients, but ultimately maintained the stance on EIP transfer as a reliable fallback. Similarly, Adams et al. [7] documented favorable long-term outcomes in seven patients following EIP to EPL transfers, with mean QuickDASH scores of 16±14, highlighting the procedure's durability.
Case reports, while inherently limited in generalizability, consistently endorse the EIP transfer approach. For instance, Patel et al. [5] detailed a successful EIP transfer in a skeletally immature patient, emphasizing the technique's adaptability across diverse patient populations. Conversely, Gelb [4] from 1995, one of the earliest comprehensive reviews, already recommended EIP transfer as the most predictable method, a stance that subsequent studies have continued to uphold.
However, alternative methods are occasionally necessitated. Fernández-Mardomingo Gutiérrez et al. [3] and Sabat et al. [9] illustrated cases where patient-specific factors precluded EIP transfer, necessitating grafting options. Additionally, the protocol by Meiwandi et al. [11] for comparing EIP and palmaris longus (PL) tendon grafting indicates ongoing research to evaluate alternative reconstruction techniques, although concrete comparative data remain forthcoming.
Complications associated with EIP transfer are infrequently reported. Adams et al. [7] and Stirling et al. [6] noted minimal adverse outcomes, aligning with Gelb’s earlier assertions regarding the procedure's safety profile [4]. However, the predominantly lower-level evidence (Levels IV and V) among case reports suggests a need for higher-level studies to robustly validate these findings and potentially uncover less common complications.
Discussion:
The extensor indicis proprius to EPL tendon transfer is consistently evidenced as an effective and reliable method for reconstructing EPL ruptures, offering significant functional restoration and patient satisfaction with minimal complications. Despite the predominance of lower-level evidence, the convergence of multiple studies and case reports supports the widespread clinical adoption of EIP transfer. Nevertheless, the limited high-level evidence underscores the necessity for more rigorous, large-scale studies to further validate these outcomes and explore alternative reconstruction techniques when EIP transfer is contraindicated.
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities




Article viewed 1560 times
15 Oct 2024
Add to Bookmarks
Full Citation
Cite this article:
230386. (2024). Extensor Indicis Proprius to Extensor Pollicis Longus Tendon Transfer for Ruptured EPL. Journal of Orthopaedic Surgery and Traumatology. Case Report 20537806 Published Online Oct 15 2024.