Sequential Anterior and Posterior ORIF in Complex Unstable Pelvic Ring Injury with Sacral Fracture and Bladder Disruption
Score and Comment on this Case
Clinical Details
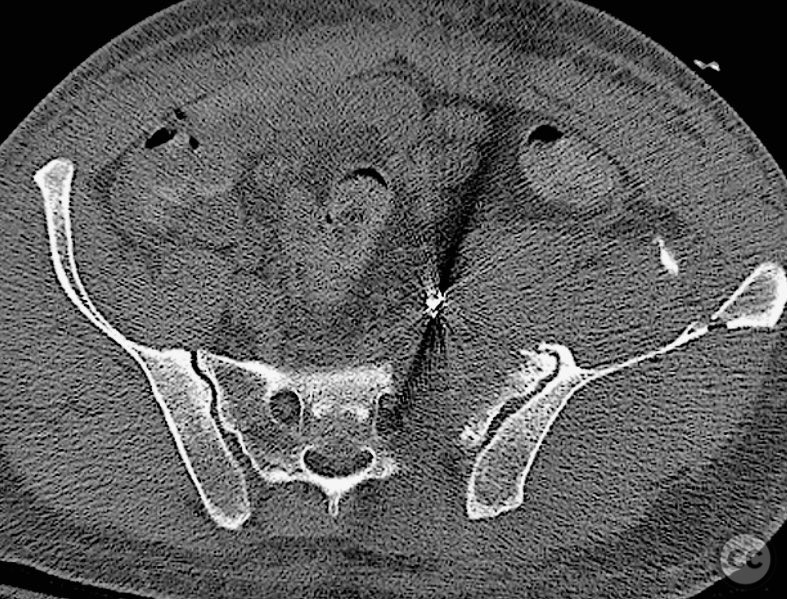
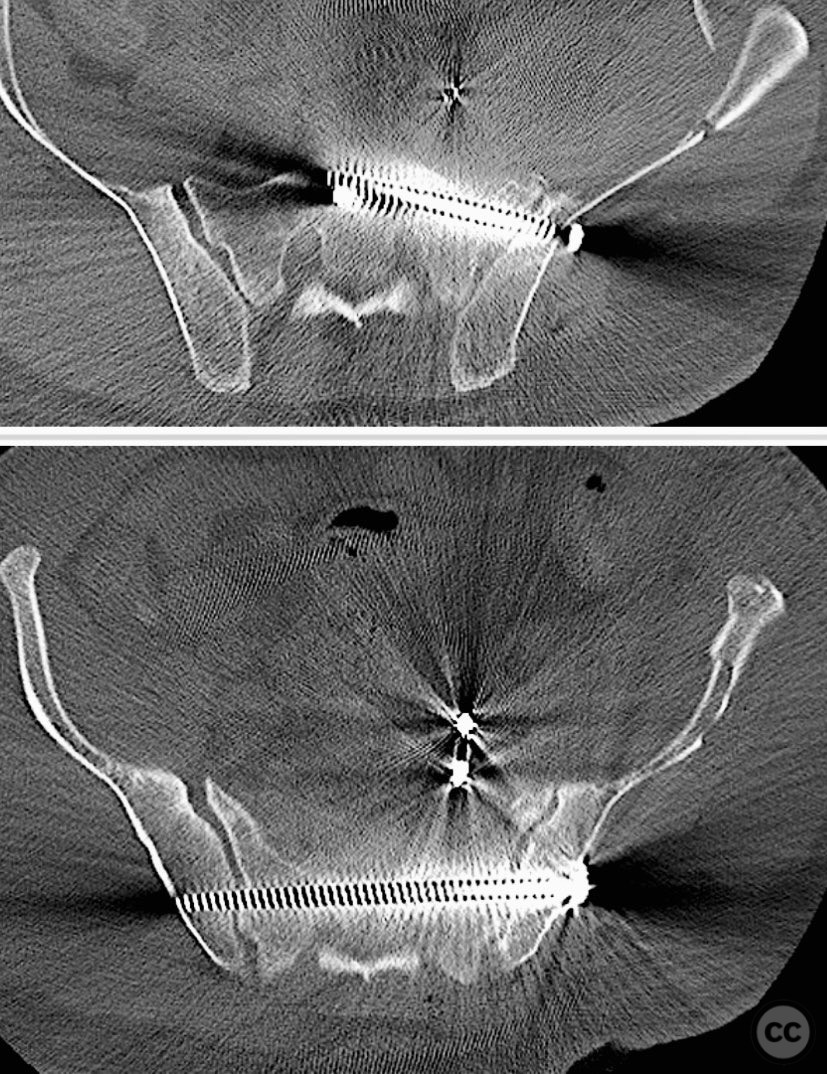
Clinical and radiological findings: A 42-year-old male sustained a high-energy motor vehicle accident resulting in an unstable pelvic ring injury (AO/OTA 61-C1.3) with hemodynamic instability and associated intraperitoneal bladder rupture. Initial computed tomography demonstrated a complex anterior pelvic ring disruption and a posterior sacral fracture with contrast extravasation and blood within the fracture site. The patient was hemodynamically unstable on presentation.
Preoperative Plan
Planning remarks: The preoperative plan included multidisciplinary management with urology for bladder repair, followed by open reduction and internal fixation of the anterior pelvic ring via an anterior approach. Subsequent posterior pelvic stabilization was planned after initial resuscitation and anterior fixation, utilizing a posterior approach for direct sacral reduction and percutaneous iliosacral screw fixation.
Surgical Discussion
Patient positioning: For anterior pelvic fixation and bladder repair, the patient was positioned supine. For posterior sacral ORIF, the patient was repositioned prone.
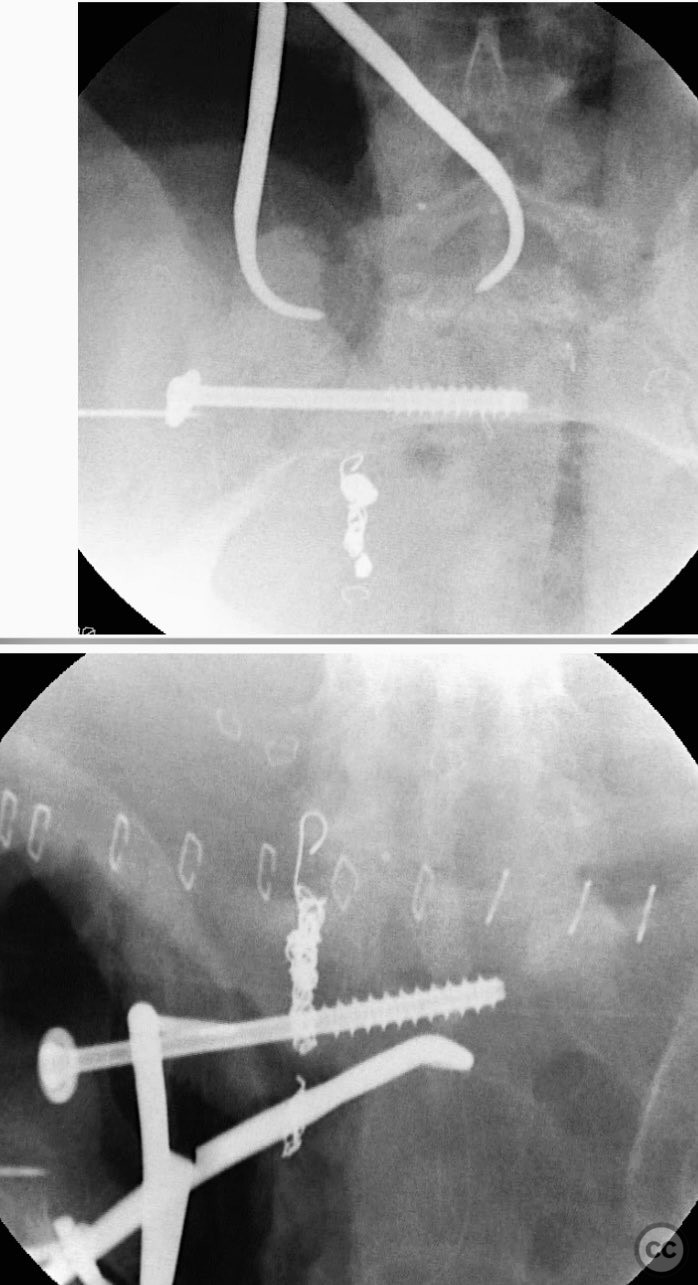
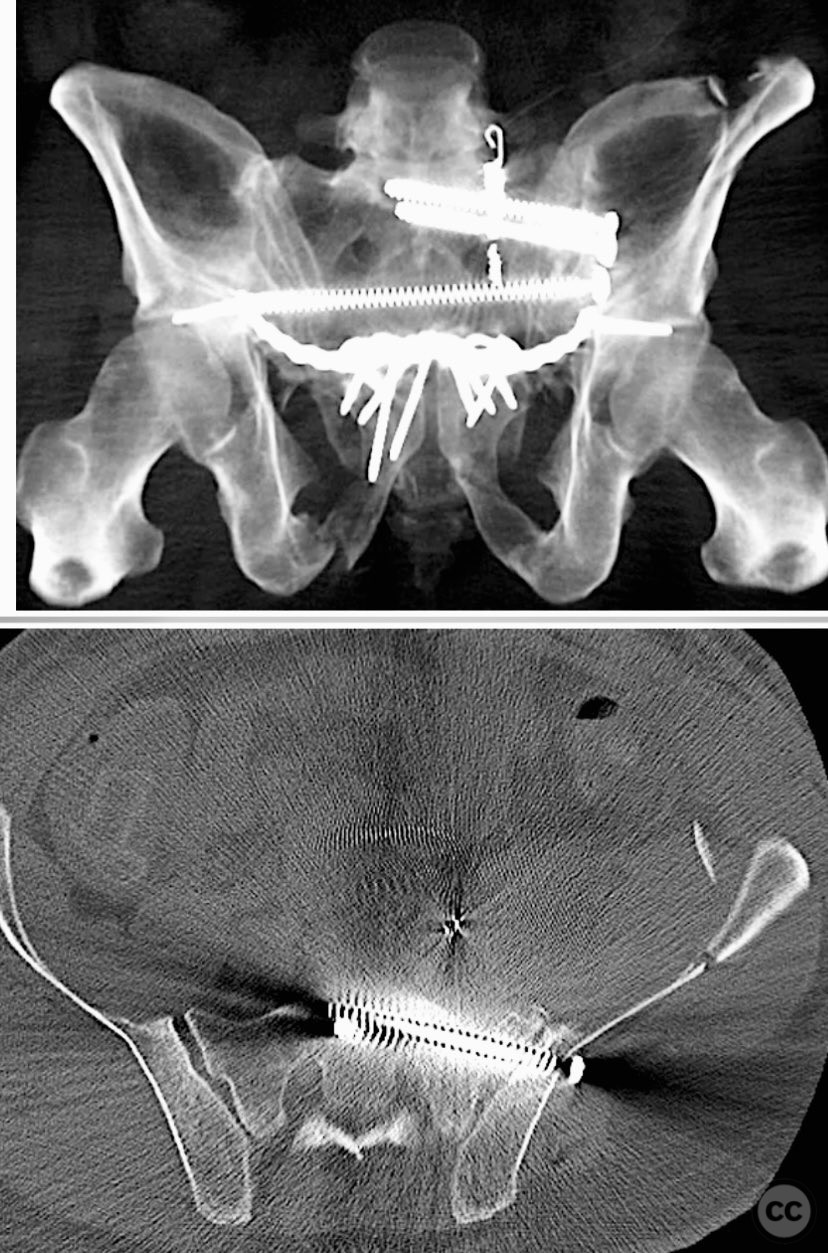
Anatomical surgical approach: The anterior approach utilized a Pfannenstiel incision to access the symphysis pubis and pubic rami, with subperiosteal dissection of the rectus abdominis and exposure of the retropubic space for reduction and fixation. For posterior sacral ORIF, a midline longitudinal incision was made over the sacrum, with subperiosteal elevation of the paraspinal musculature to expose the sacral fracture. A tenaculum clamp was applied for direct reduction, followed by percutaneous insertion of iliosacral screws under fluoroscopic guidance.
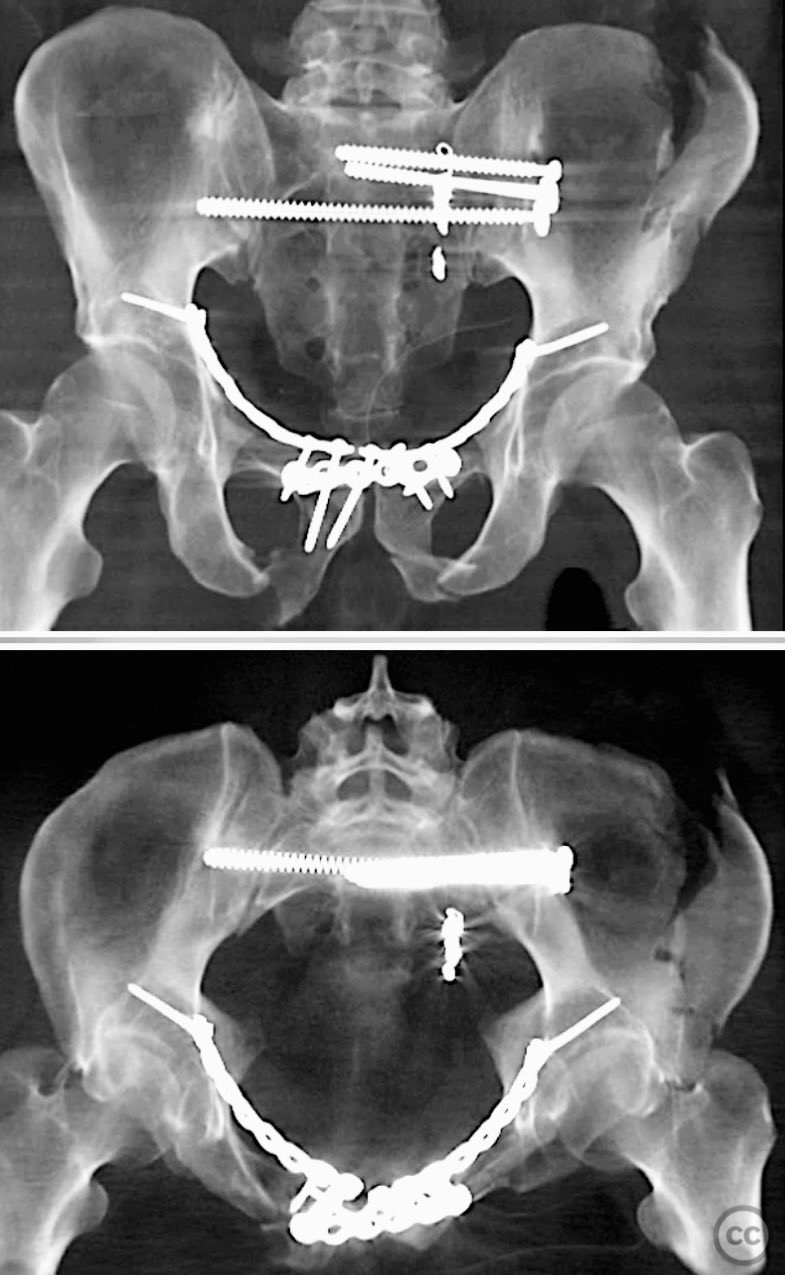
Operative remarks:The case was notable for initial successful multidisciplinary management of both hemodynamic instability and intraperitoneal bladder injury, allowing for staged surgical intervention. Despite accurate anterior pelvic reduction and fixation, postoperative imaging revealed worsening posterior sacral displacement, necessitating subsequent posterior open reduction. The use of a tenaculum clamp facilitated direct anatomical reduction of the sacral fracture prior to iliosacral screw fixation. The presence of an embolic coil from prior angioembolization did not impede surgical access or hardware placement. This case demonstrates that initial anterior pelvic ORIF does not complicate or preclude subsequent routine posterior pelvic ORIF in complex unstable ring injuries.
Postoperative protocol: Postoperative protocol included restricted weight bearing for 8 weeks, early passive range of motion exercises for the lower extremities, and progressive mobilization as tolerated after radiographic evidence of healing.
Follow up: Not specified
Orthopaedic implants used: Anterior pelvic reconstruction plate, iliosacral cannulated screws, tenaculum reduction clamp
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities




Article viewed 152 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Sequential Anterior and Posterior ORIF in Complex Unstable Pelvic Ring Injury with Sacral Fracture and Bladder Disruption. Journal of Orthopaedic Surgery and Traumatology. Case Report 19367863 Published Online Sep 11 2025.