High-energy segmental tibia fracture with vascular injury and severe soft tissue compromise.
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: A 29-year-old male involved in a high-speed motorcycle collision presented with an 8 cm open posteromedial wound at the knee and a medial pokehole wound at the distal tibia. The patient was transferred with a tourniquet applied for 4 hours, following a 2-hour delay post-injury. On arrival, the patient had no palpable pulses and had experienced a pulseless electrical activity (PEA) arrest en route, with spontaneous return of circulation after CPR. Initial laboratory findings included a lactate level of 4.5 mmol/L and a hematocrit of 22%. Bilateral chest tubes were placed for hemopneumothorax. Computed Tomography Angiography (CTA) revealed a vascular injury at the trifurcation with occlusion of all three vessels. The injury was classified as a Gustilo-Anderson type IIIC open fracture with segmental tibial involvement and significant soft tissue damage.
Preoperative Plan
Planning remarks: The preoperative plan involved immediate coordination with vascular surgery for shunting of the injured vessels, followed by orthopaedic intervention. The orthopaedic plan included performing fasciotomies to address compartment syndrome, applying an external fixator to maintain limb length, and provisional plating of the proximal tibial fracture.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table to facilitate simultaneous vascular and orthopaedic interventions.
Anatomical surgical approach: A medial approach to the tibia was utilized for fasciotomy and debridement of devitalized tissue. An external fixator was applied to maintain limb length and alignment. Provisional plating of the proximal tibial fracture was performed through a separate incision.
Operative remarks:The operative course required close coordination between surgical teams due to the patient’s critical condition and complex injury pattern.
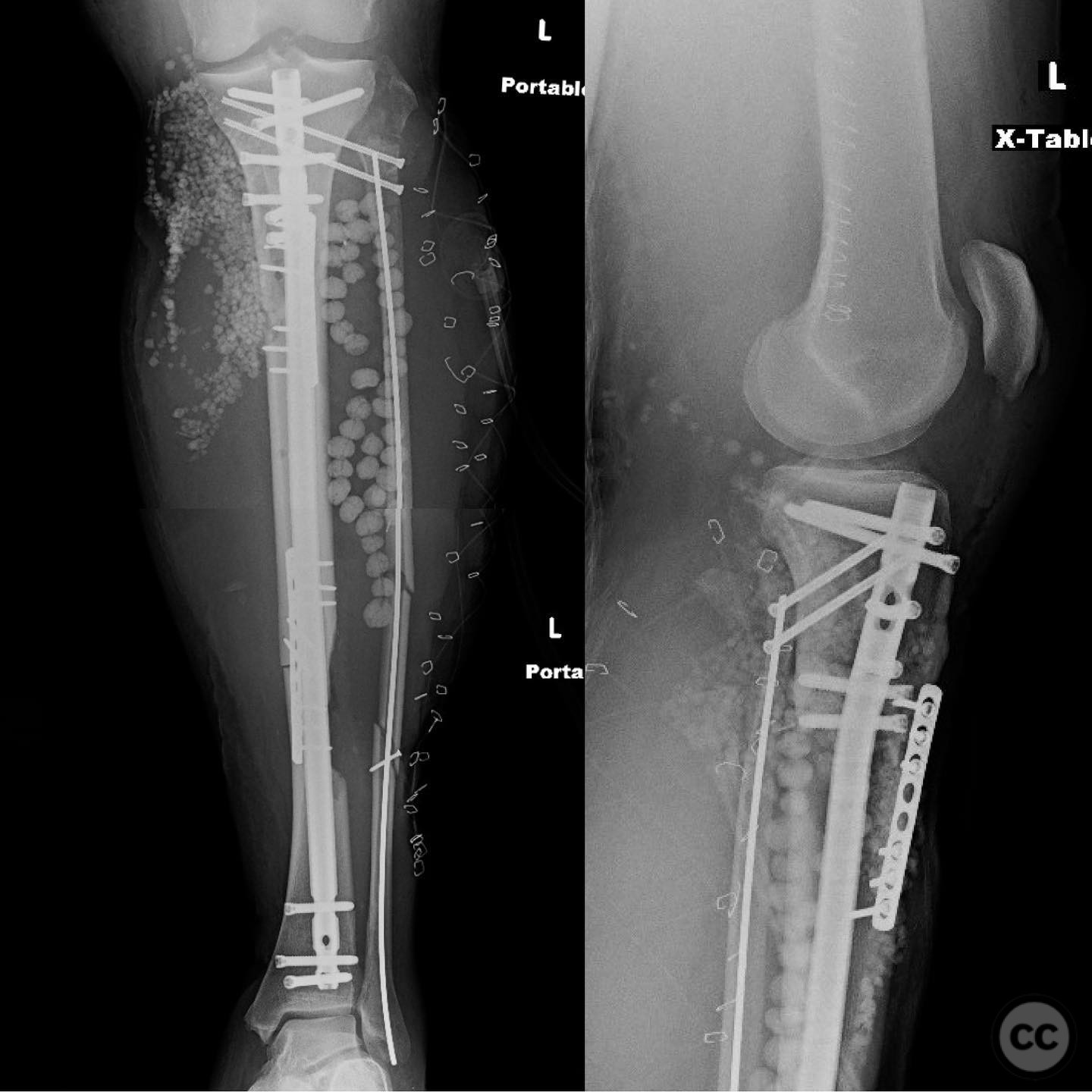
Initial imaging showed complete occlusion of all three trifurcation vessels. A temporary vascular shunt was placed, followed by four-compartment fasciotomies and external fixation to restore limb length. The shunt was later replaced with an interposition graft, and the proximal tibial fracture was provisionally plated.
After stabilization, the patient was transferred to the ICU.
A second-look procedure the following day included further debridement, provisional plating of the distal tibia, and fibular fixation using intramedullary nailing and pinning due to marked distraction at the fracture site.
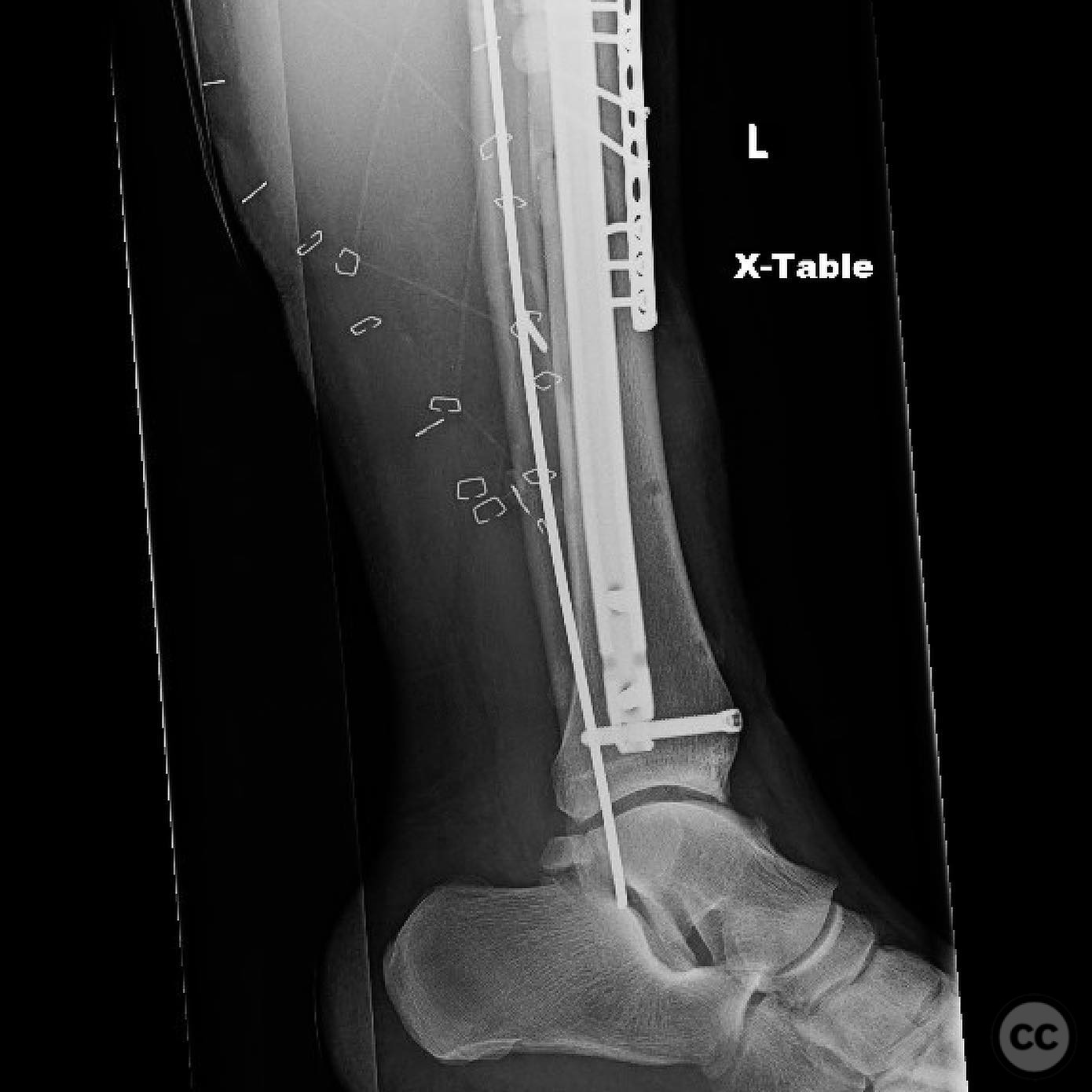
Definitive fixation was completed after confirming soft tissue viability, using tibial intramedullary nailing and screw fixation of the proximal segment.
Postoperative protocol: Postoperative rehabilitation included early transfer to the ICU for hemodynamic stabilization and serial debridements. Weight-bearing status was initially restricted, with gradual progression based on soft tissue healing and vascular status.
Follow up: Not specified.
Orthopaedic implants used: External fixator, provisional plates for proximal and distal tibia, intramedullary nail for tibia, pins for fibula stabilization.
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities












Article viewed 187 times
12 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). High-energy segmental tibia fracture with vascular injury and severe soft tissue compromise.. Journal of Orthopaedic Surgery and Traumatology. Case Report 18018541 Published Online Jul 12 2025.