Comminuted Posterior Wall Acetabular Fracture-Dislocation with Greater Sciatic Notch Involvement and Sciatic Nerve Impalement
Score and Comment on this Case
Clinical Details
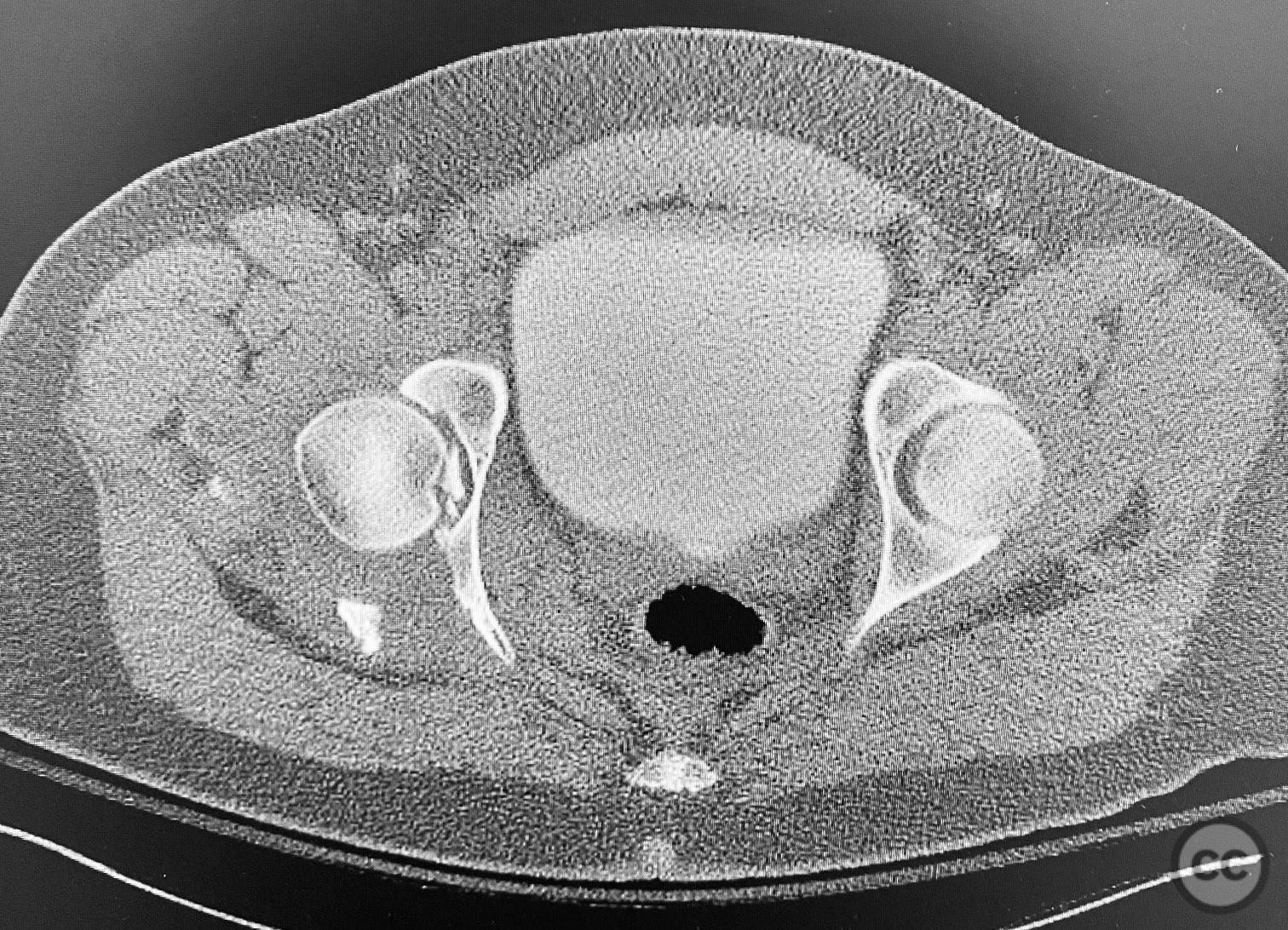
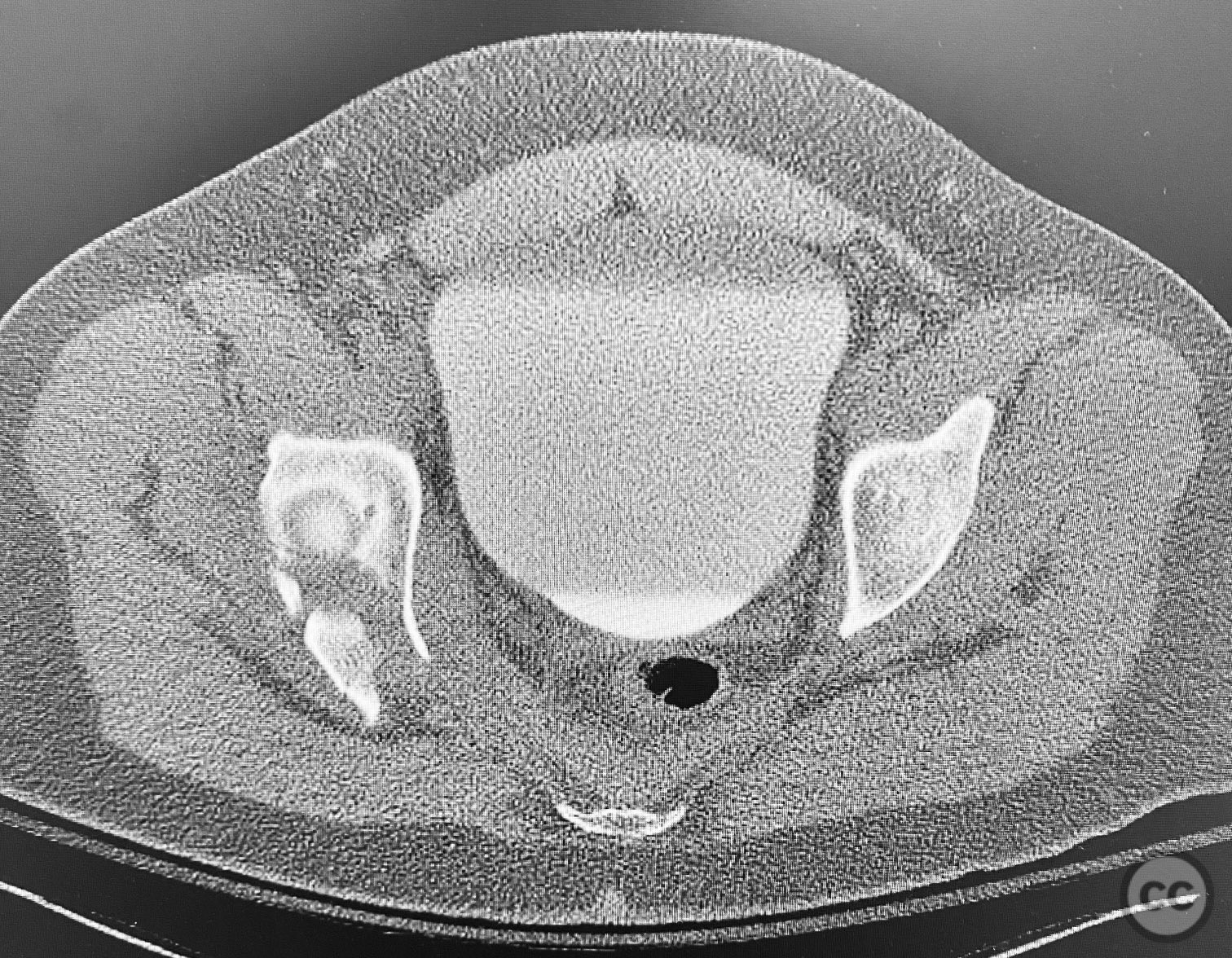
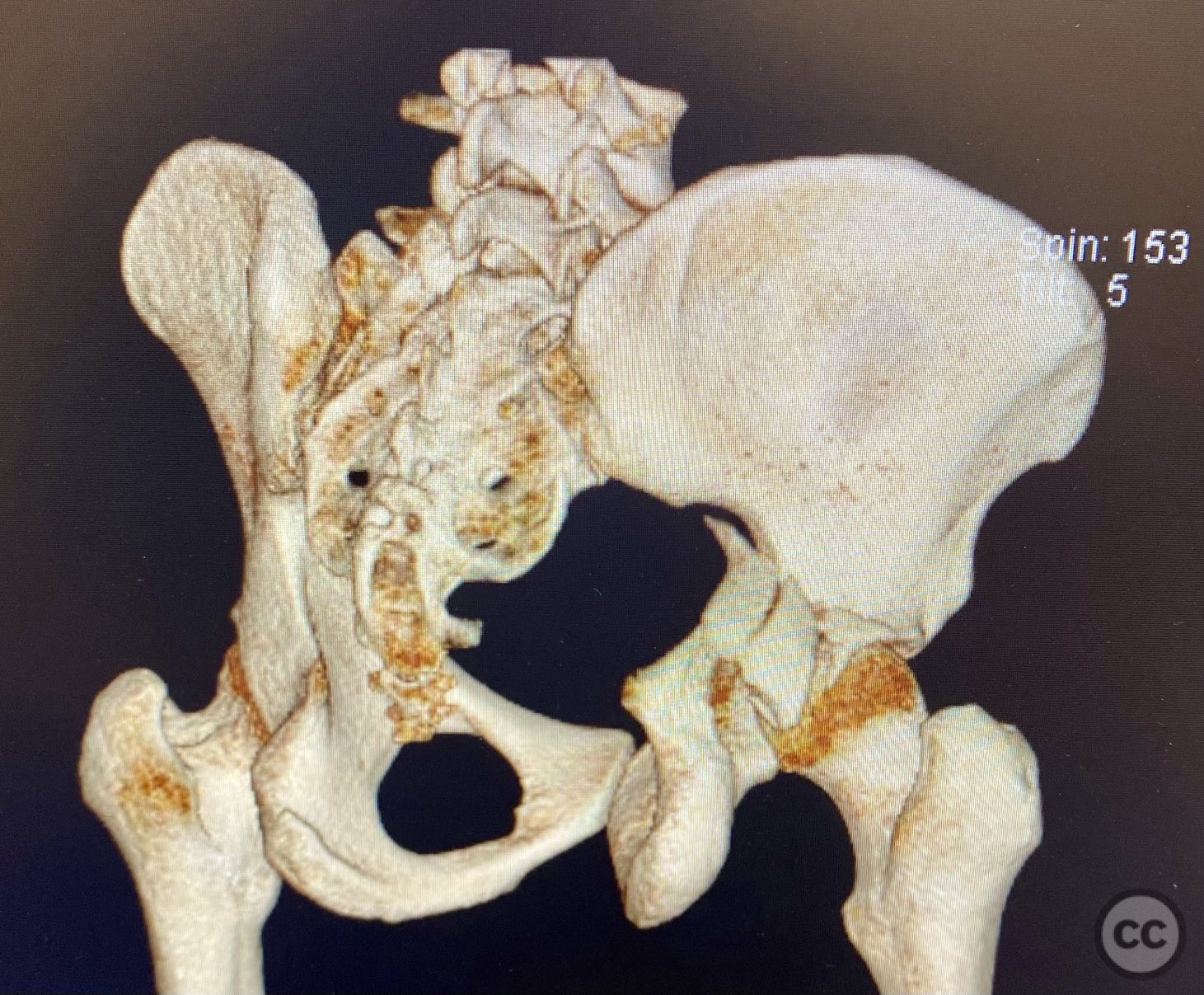
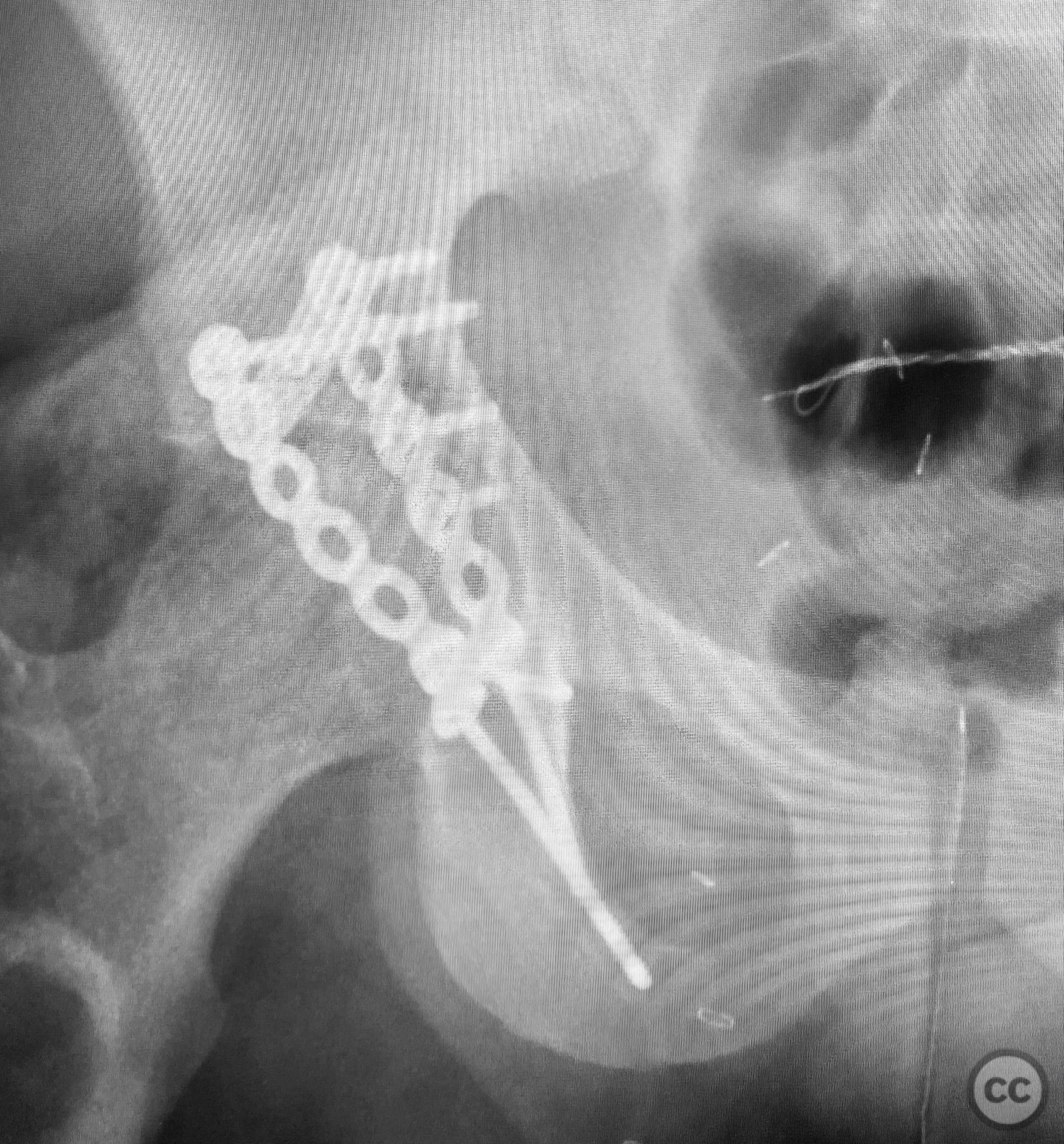
Clinical and radiological findings: A patient sustained a comminuted posterior wall acetabular fracture-dislocation (AO/OTA 62-B1.3) involving the greater sciatic notch, with associated traumatic sciatic nerve injury. Following closed reduction, imaging demonstrated an intra-articular fragment located within the acetabular fossa (fossa acetabuli). Clinical examination revealed neurological deficit consistent with sciatic nerve involvement. Radiographs and CT confirmed the extent of comminution and intra-articular displacement.
Preoperative Plan
Planning remarks: The preoperative plan included a Kocher-Langenbeck (KL) approach in the prone position for open reduction and internal fixation of the posterior wall fragments, removal and reduction of the intra-articular fossa fragment, and exploration of the sciatic nerve with neuroplasty. Fixation was planned using a combination of standard plates and a spring hook plate to address the cranial wall fragment.
Surgical Discussion
Patient positioning: The patient was positioned prone on a radiolucent table, with appropriate padding to protect pressure points and facilitate posterior pelvic access.
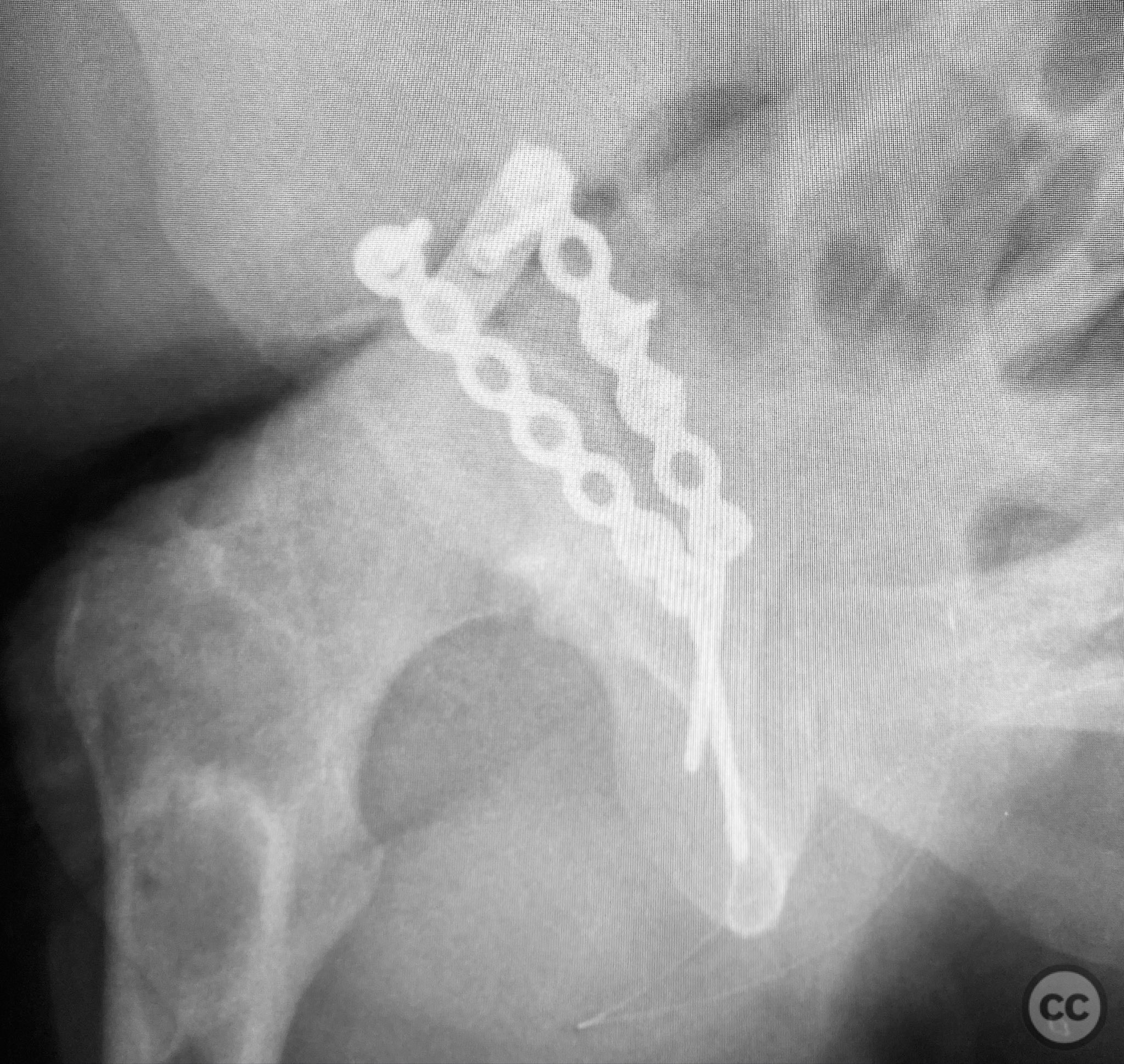
Anatomical surgical approach: A standard Kocher-Langenbeck approach was performed: a longitudinal incision centered over the greater trochanter, extending proximally along the posterior iliac crest and distally along the femoral shaft. The fascia lata was incised, and the gluteus maximus split in line with its fibers. The short external rotators and piriformis were identified, tagged, and released to expose the posterior column and wall of the acetabulum. The sciatic nerve was identified in the greater sciatic notch region; intraoperatively, it was found to be severely contused, displaced, and uniquely penetrated by a sharp posterior wall fragment. Neuroplasty was performed, freeing the nerve from impalement and surrounding scar tissue. The intra-articular fossa acetabuli fragment was extracted, anatomically reduced, and stabilized along with other posterior wall fragments. A spring hook plate was applied to secure the cranial wall fragment due to its size and comminution.
Operative remarks:Intraoperatively, the sciatic nerve was found to be not only contused but also impaled by a displaced posterior wall fragment—a rare occurrence in acetabular trauma. Careful neuroplasty was required to release the nerve from direct bony penetration without further iatrogenic injury. Reduction of all articular fragments was achieved under direct visualization, with particular attention to restoring congruity of the acetabular rim and fossa. The use of a spring hook plate provided necessary buttress for the large cranial wall fragment, which could not be adequately stabilized with standard plating alone.
Postoperative protocol: Postoperatively, the patient was maintained non-weight bearing on the affected limb for 8 weeks. Passive range of motion exercises were initiated immediately, avoiding excessive hip flexion (>60°) for 6 weeks to protect the repair. Progressive weight bearing was introduced after radiographic evidence of healing at 8–10 weeks. Neurological function was monitored closely, with referral to physiotherapy for both hip rehabilitation and neuro-recovery protocols.
Follow up: Not specified
Orthopaedic implants used: 3.5mm reconstruction plate, spring hook plate
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities




Article viewed 90 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Comminuted Posterior Wall Acetabular Fracture-Dislocation with Greater Sciatic Notch Involvement and Sciatic Nerve Impalement. Journal of Orthopaedic Surgery and Traumatology. Case Report 16573533 Published Online Sep 11 2025.