Percutaneous CurvaFix Fixation of Oblique Upper Sacral Fracture in Elderly Patient
Score and Comment on this Case
Clinical Details
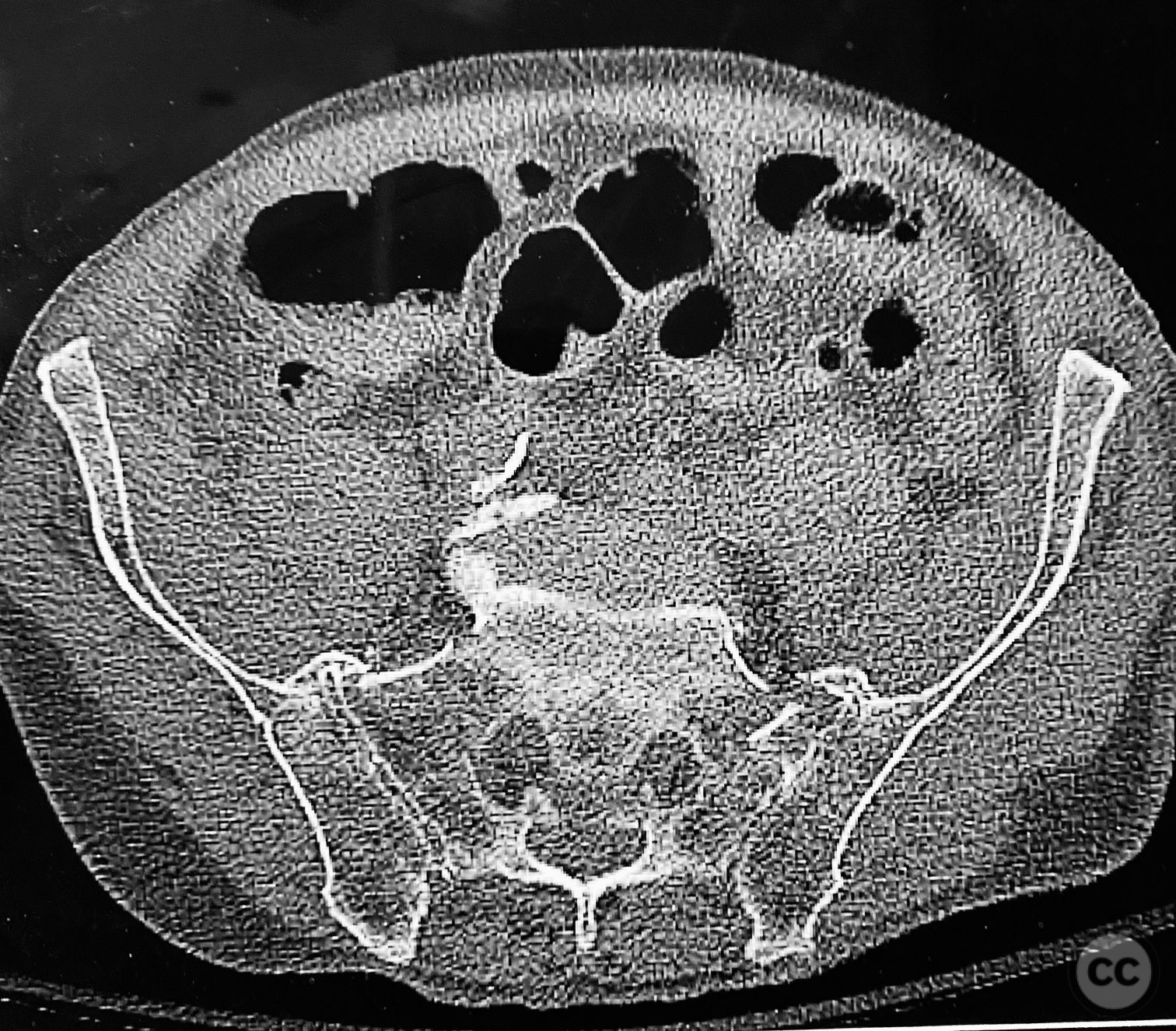
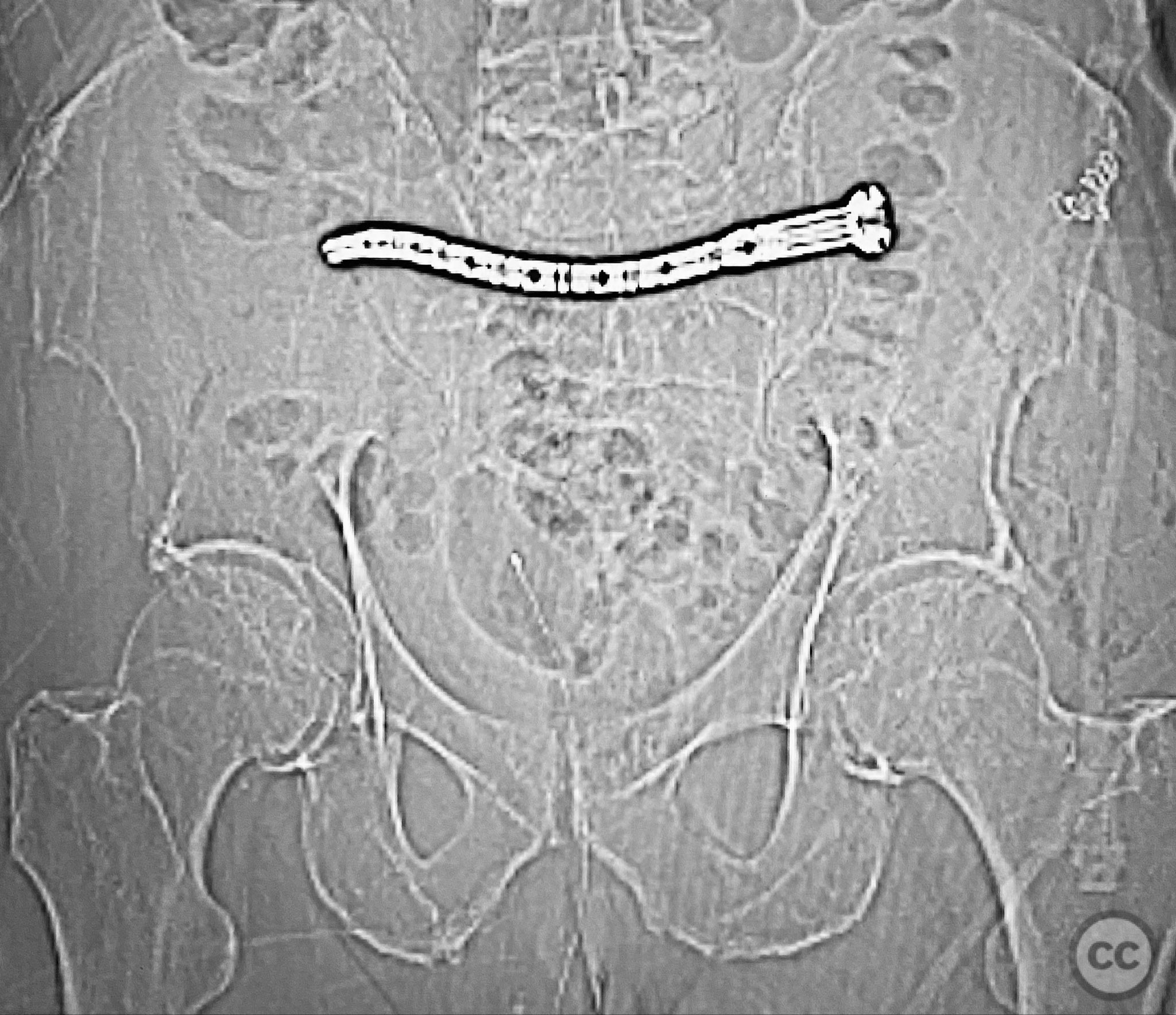
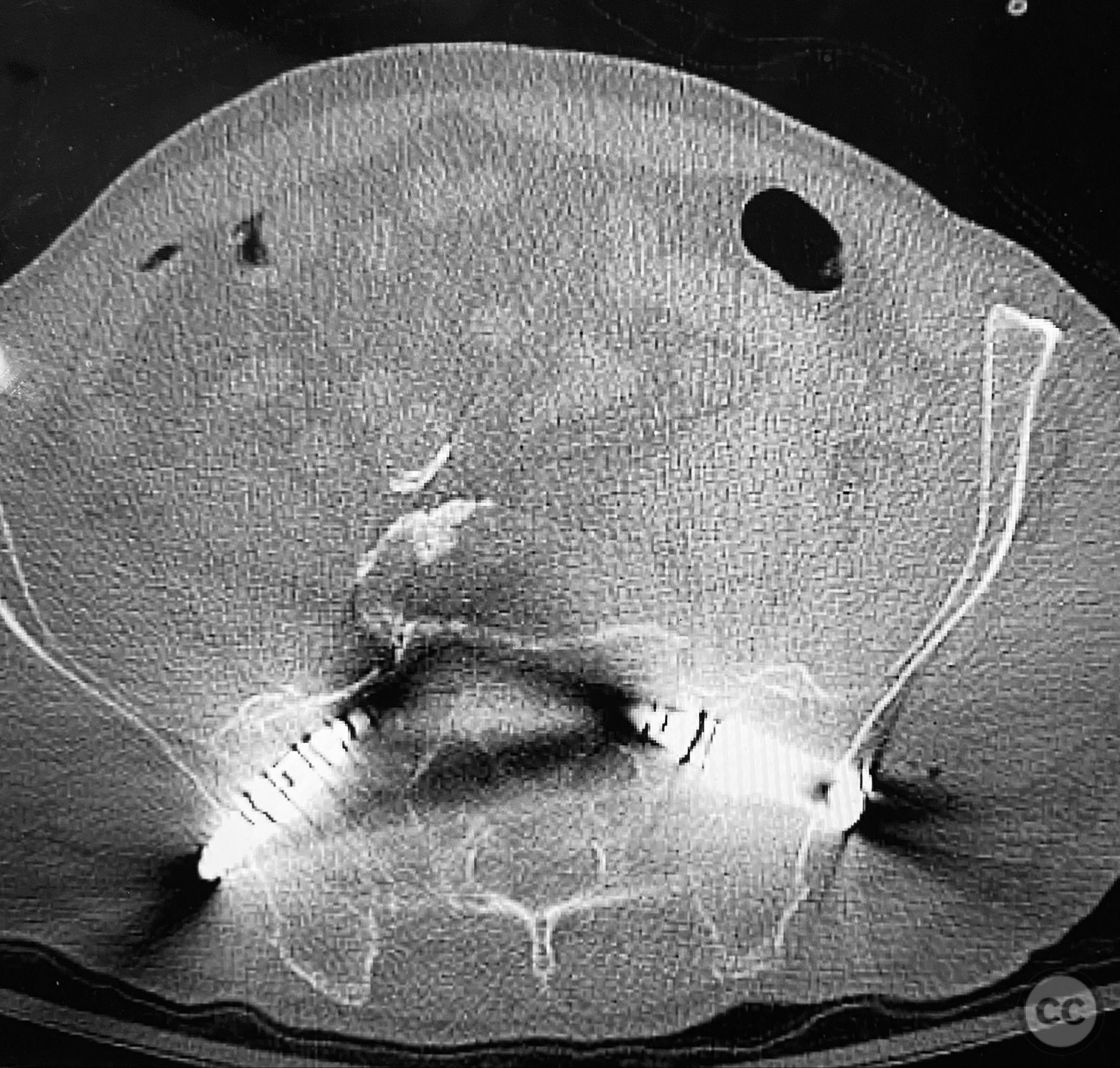
Clinical and radiological findings: An elderly patient presented with a complex upper sacral fracture characterized by oblique fracture pathways bilaterally, described as a "UYH+pattern" fracture. The patient exhibited compromised bone quality consistent with age-related osteopenia or osteoporosis. Initial clinical assessment prioritized pain control and early mobilization. Radiological evaluation, including computed tomography (CT), confirmed the oblique orientation of the upper sacral fracture lines and their bilateral extension. No neurovascular compromise was reported.
Preoperative Plan
Planning remarks: The preoperative plan involved percutaneous stabilization of the bilateral oblique upper sacral fractures using a cannulated, articulated intramedullary fixation device (CurvaFix). The anatomical approach was planned to accommodate the oblique trajectory of the sacral fracture pathways, with bilateral guide pin placement under fluoroscopic guidance, followed by device insertion and locking.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent operating table to facilitate fluoroscopic imaging in multiple planes (anteroposterior, inlet, and outlet views) for accurate guide pin and device placement.
Anatomical surgical approach: Percutaneous access was established over the dorsal aspect of the pelvis. Small incisions were made lateral to the sacrum, and soft tissue dissection was performed to the level of the os sacrum. Guide pins were advanced under fluoroscopic control along the oblique upper sacral corridors bilaterally. The cannulated CurvaFix device was inserted over each guide pin, articulated to match the oblique fracture pathway, and subsequently locked in situ according to the manufacturer’s specifications.
Operative remarks:The articulated nature of the CurvaFix device allowed precise accommodation of the complex oblique upper sacral fracture pathways bilaterally. Percutaneous technique minimized soft tissue disruption and surgical morbidity. Postoperative CT imaging confirmed satisfactory device placement and fracture reduction. The achieved stability provided immediate pain relief, reduced or eliminated narcotic requirements, and enabled early mobilization. Surgeons with experience in device removal have reported no technical difficulties.
Postoperative protocol: Early mobilization was initiated postoperatively as tolerated by the patient, with weight bearing as permitted by comfort and stability. Standard deep vein thrombosis prophylaxis and physiotherapy were instituted. No external immobilization was required.
Follow up: Not specified
Orthopaedic implants used: CurvaFix intramedullary fixation device
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities




.jpg)

Article viewed 129 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Percutaneous CurvaFix Fixation of Oblique Upper Sacral Fracture in Elderly Patient. Journal of Orthopaedic Surgery and Traumatology. Case Report 16009471 Published Online Sep 11 2025.