Posterior Wall Acetabular Fracture-Dislocation with Comminution, Impaction, and Intra-articular Fragments
Score and Comment on this Case
Clinical Details
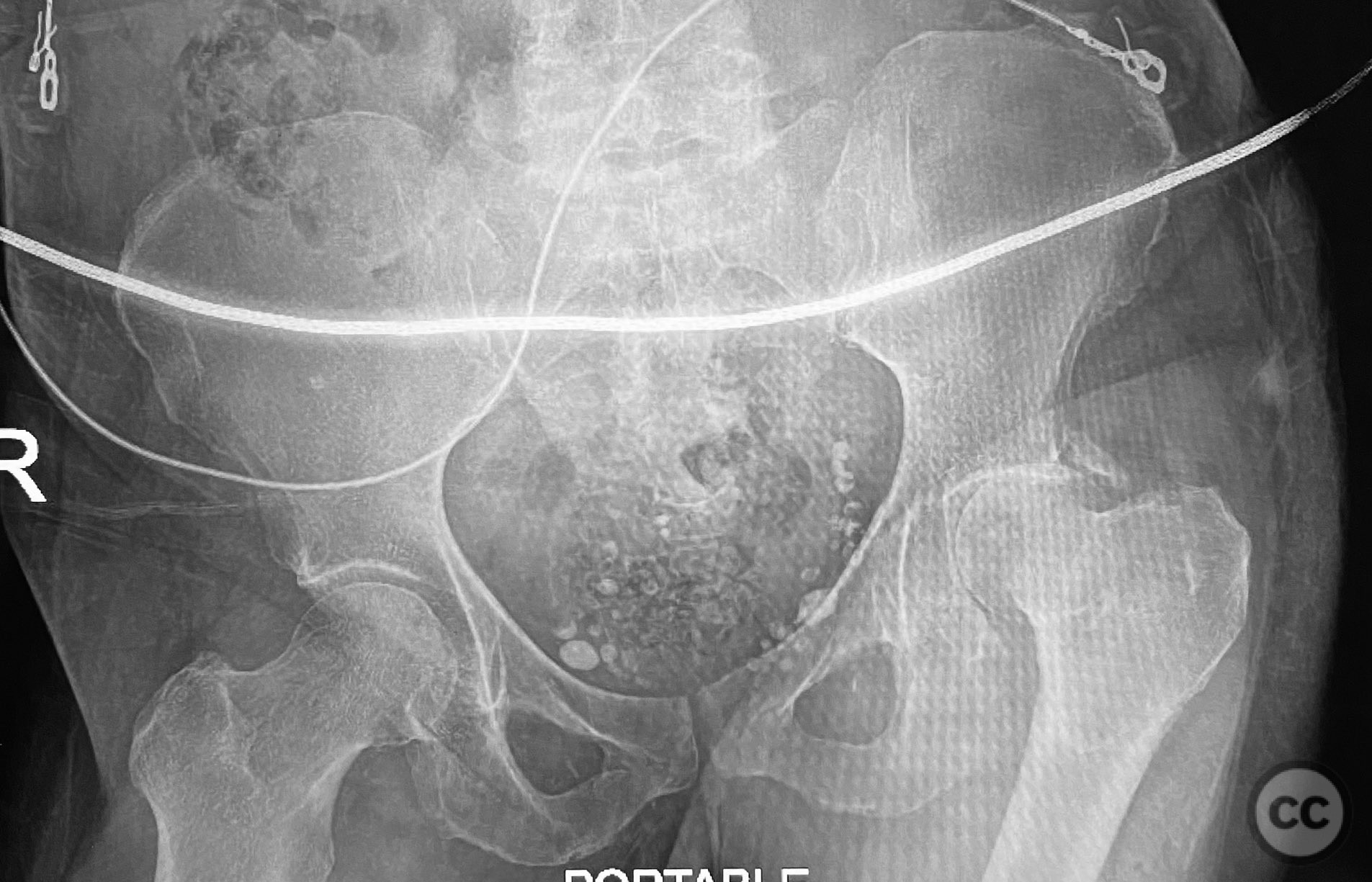
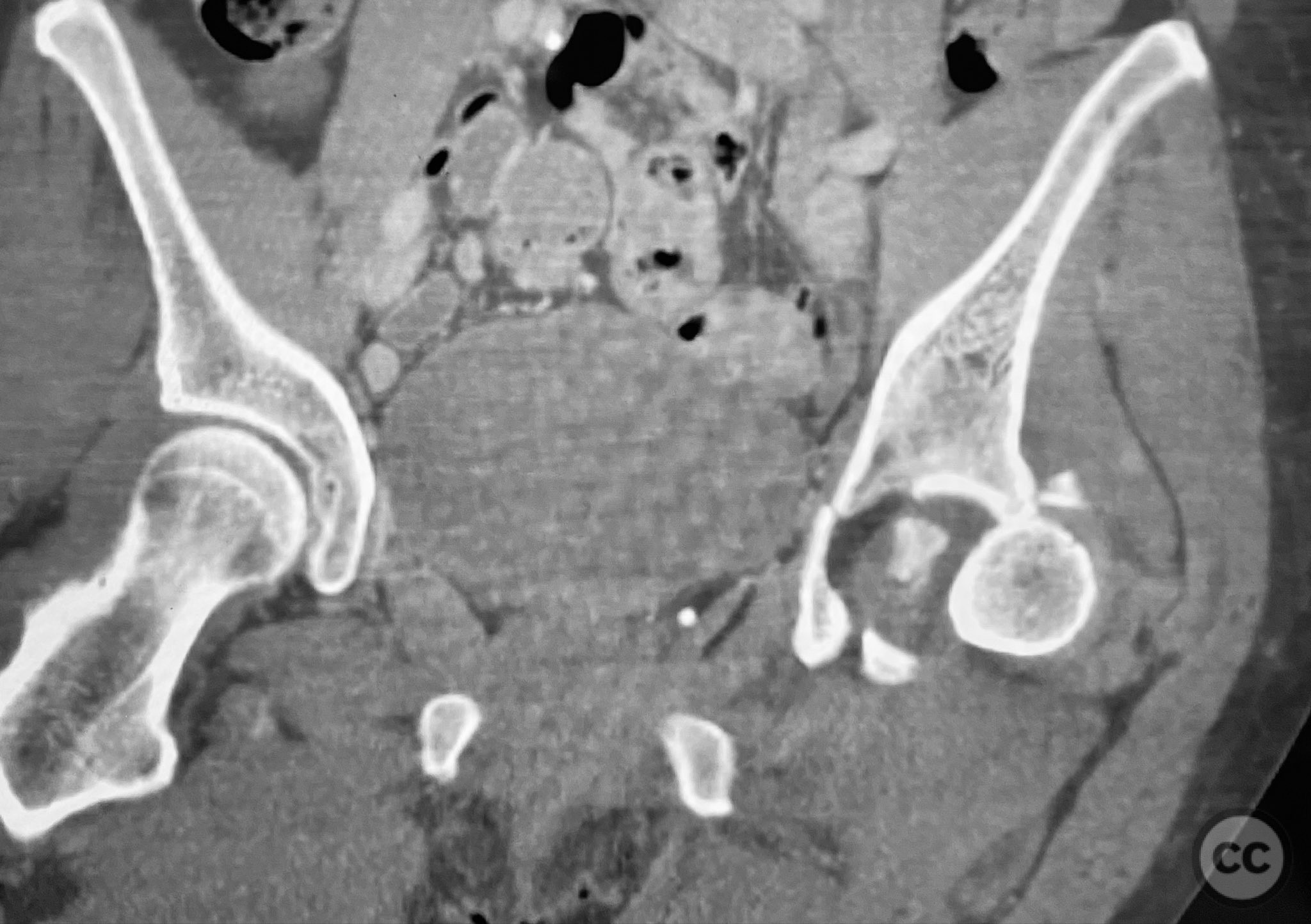
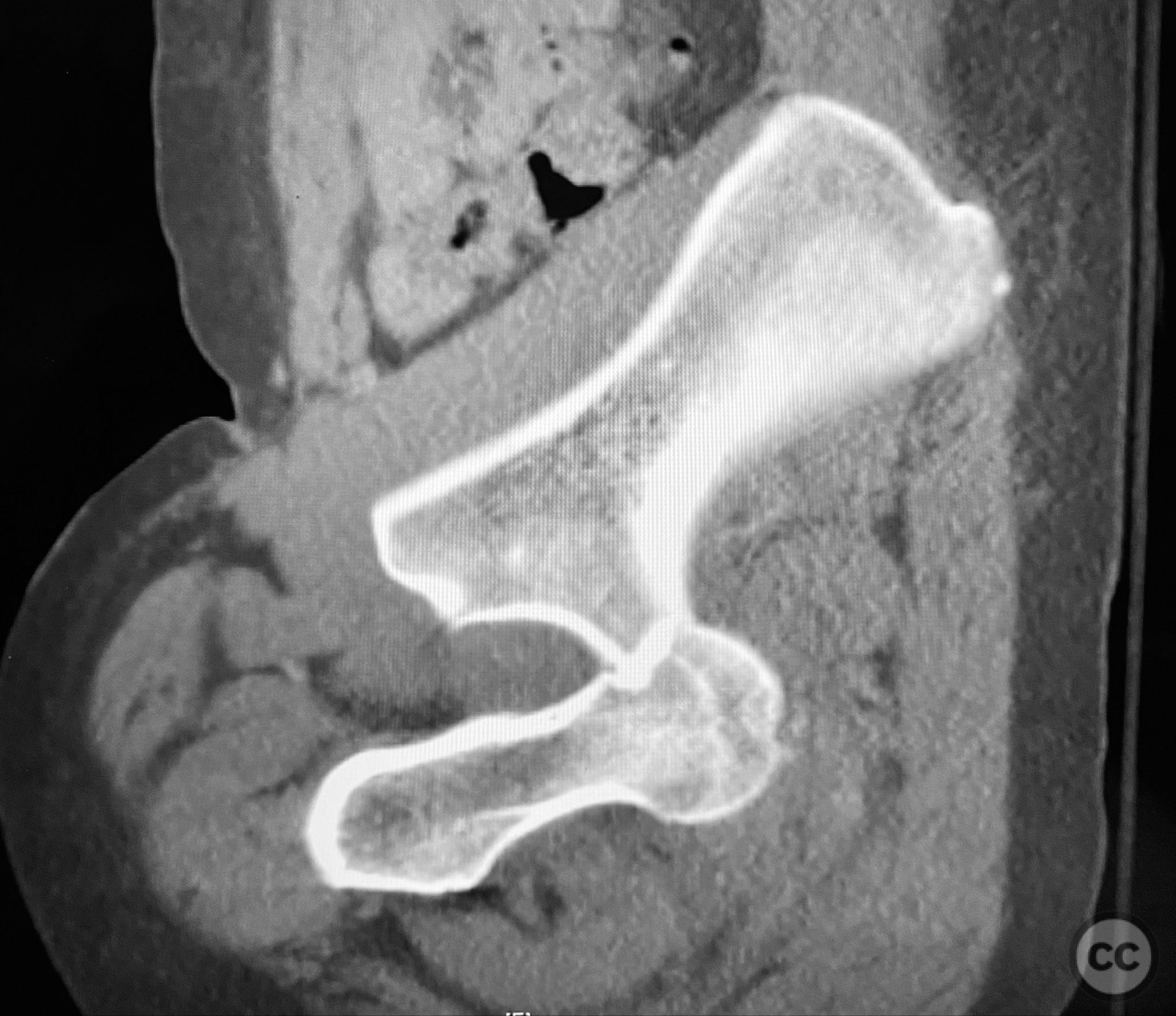
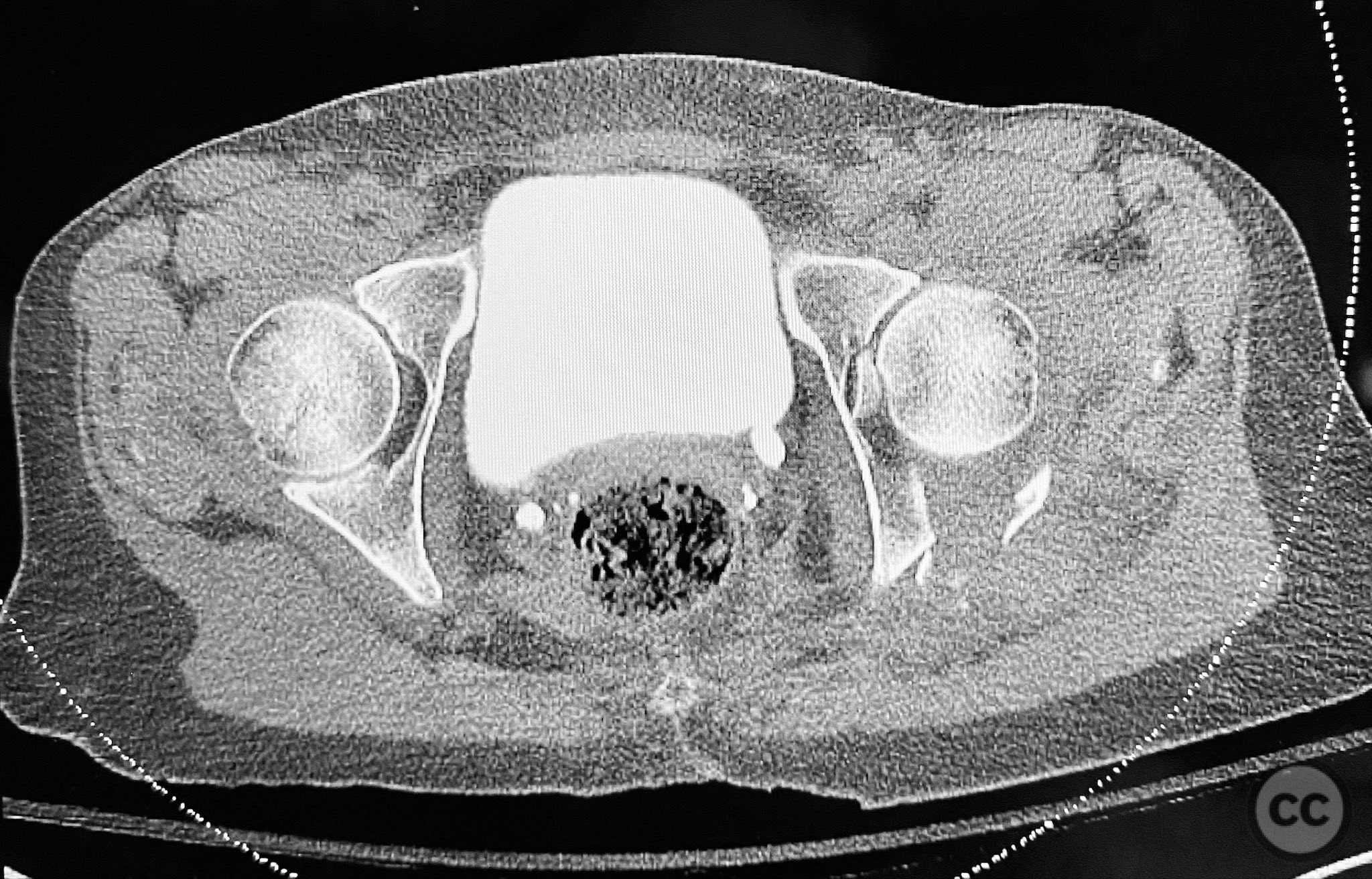
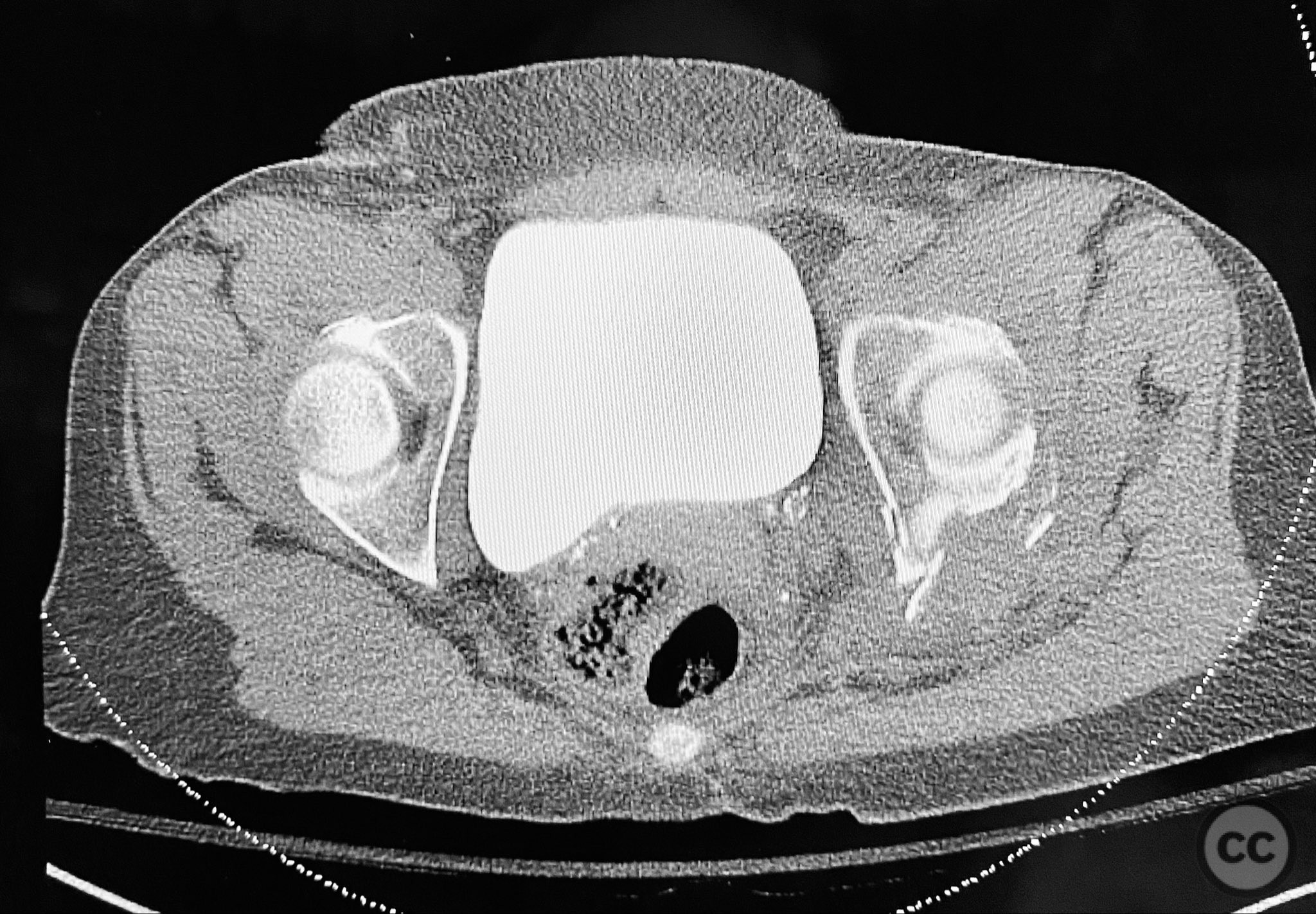
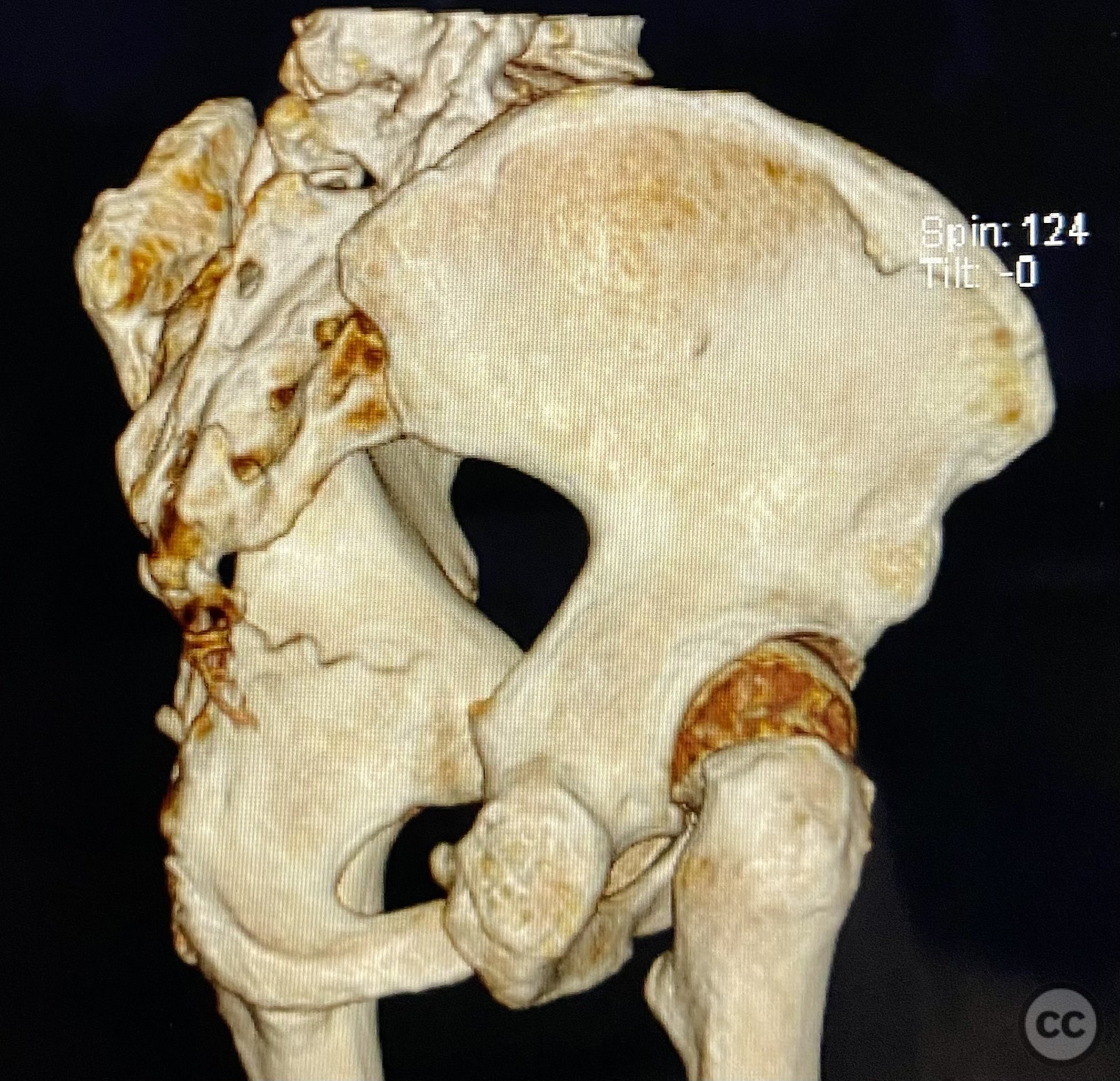
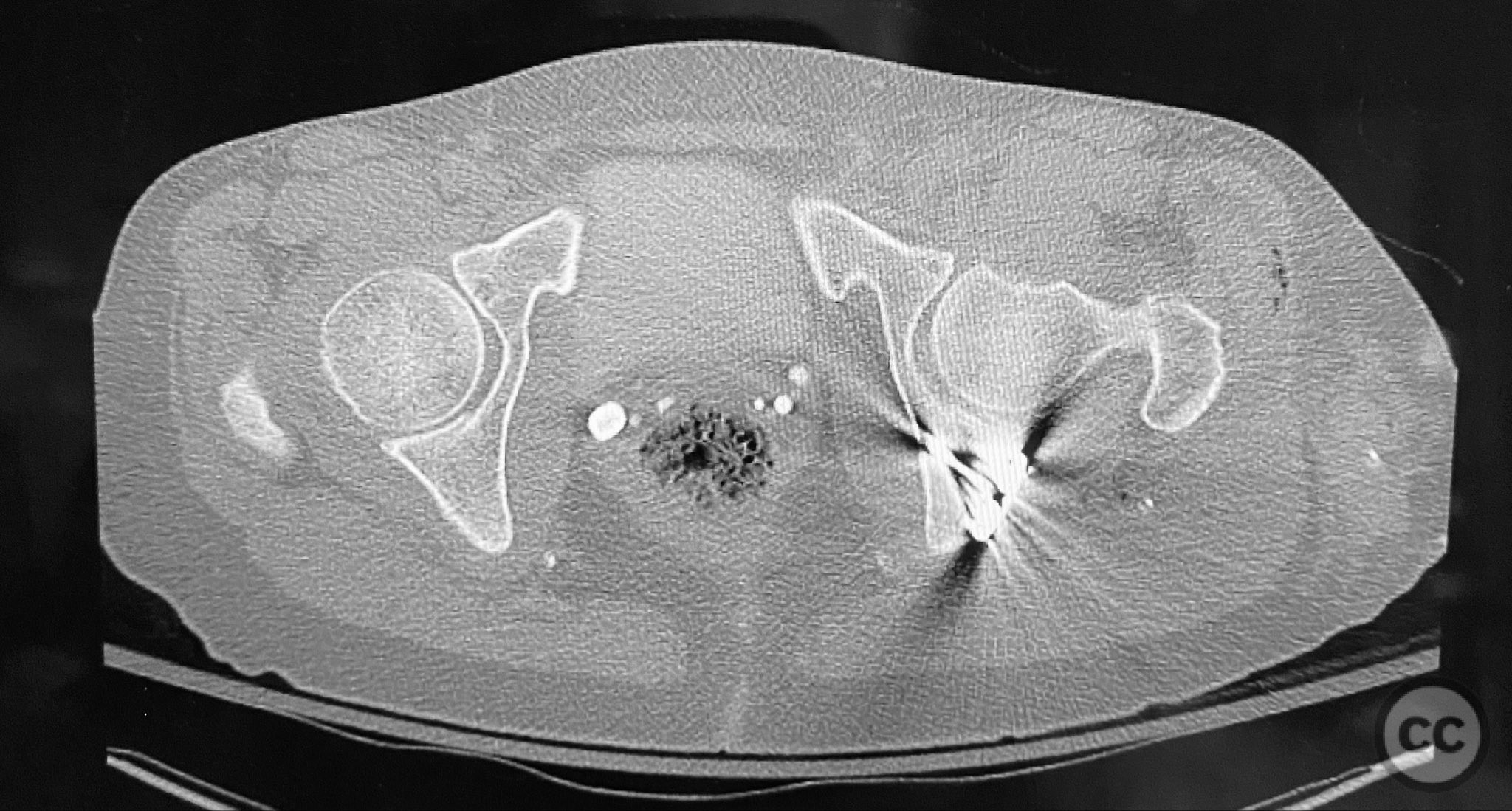
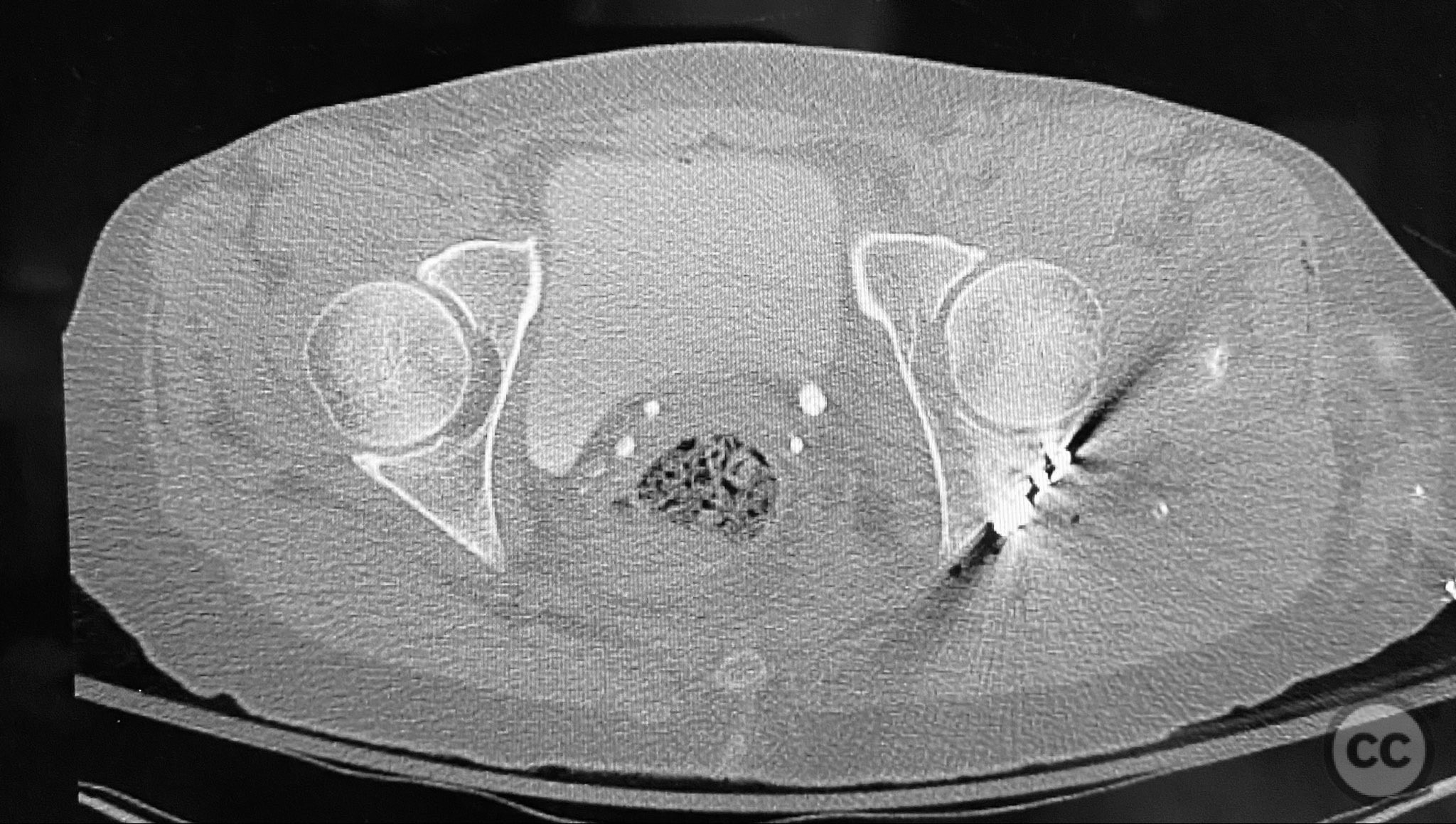
Clinical and radiological findings: A patient sustained a posterior wall acetabular fracture-dislocation, characterized by comminution of the posterior wall, impaction of fragments into the posterior column region, and intra-articular loose fragments within the fossa acetabuli. Sagittal imaging demonstrated femoral head impalement on the intact wall, raising concern for potential irreducibility. Coronal and axial CT images revealed acetabular and femoral head impactions, peripheral wall comminution, incomplete fracture extension at the acetabular notch and quadrilateral surface, and an articular fragment within the joint. Surface renderings confirmed the extent of peripheral wall comminution and impaction. Despite these findings, a closed manipulative reduction was successfully achieved, resulting in a congruent reduction on post-reduction imaging.
Preoperative Plan
Planning remarks: The preoperative plan included a prone Kocher-Langenbeck (KL) approach to the acetabulum. The plan involved application of a distractor to facilitate removal of intra-articular loose fragments, elevation of impacted articular segments, bone grafting of resultant defects with ground allograft, and stabilization of the posterior wall with multiple plates, including a custom spring hook plate for peripheral fragment support.
Surgical Discussion
Patient positioning: The patient was positioned prone on a radiolucent table to facilitate posterior access to the acetabulum via the Kocher-Langenbeck approach.
Anatomical surgical approach: A standard Kocher-Langenbeck approach was performed with a longitudinal incision centered over the greater trochanter, extending proximally along the axis of the gluteus maximus and distally along the femoral shaft. The gluteus maximus was split in line with its fibers, and the short external rotators were detached from their femoral insertions and retracted medially to expose the posterior column and wall of the acetabulum. The sciatic nerve was identified and protected throughout. A distractor was applied across the hip joint to facilitate joint distraction and removal of intra-articular fragments. Impacted articular fragments were elevated, and defects were grafted with ground allograft. Posterior wall fragments were anatomically reduced and stabilized with a combination of plates: a lateral reconstruction plate, a standard buttress plate, and a custom spring hook plate fashioned from a third tubular plate with tines contoured to engage the cortical surface of the posterior wall fragment. The central hole of the spring hook plate was filled first to provide spring tension, followed by fixation of the medial hole to secure the implant.
Operative remarks:The injury demonstrated extensive comminution and impaction of the posterior wall with intra-articular debris requiring meticulous removal and elevation. The use of a distractor facilitated both exposure and removal of loose articular fragments. The peripheral comminution necessitated augmentation with a custom spring hook plate to maintain reduction of small cortical fragments not amenable to standard buttress plating. Proper placement of the lateral reconstruction plate overlying the spring hook plate was critical for maintaining fixation integrity; malpositioning resulted in early fixation failure in a comparative case due to bending of the unsupported spring hook implant.
Postoperative protocol: Postoperatively, toe-touch weight bearing was instituted for 8–12 weeks with passive and active-assisted range-of-motion exercises initiated immediately. Progressive weight bearing was allowed after radiographic evidence of healing at 8–12 weeks.
Follow up: Not specified
Orthopaedic implants used: 3.5 mm reconstruction plate, standard buttress plate, custom spring hook plate (fashioned from third tubular plate), ground allograft
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities










Article viewed 156 times
12 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Posterior Wall Acetabular Fracture-Dislocation with Comminution, Impaction, and Intra-articular Fragments. Journal of Orthopaedic Surgery and Traumatology. Case Report 14661840 Published Online Sep 12 2025.