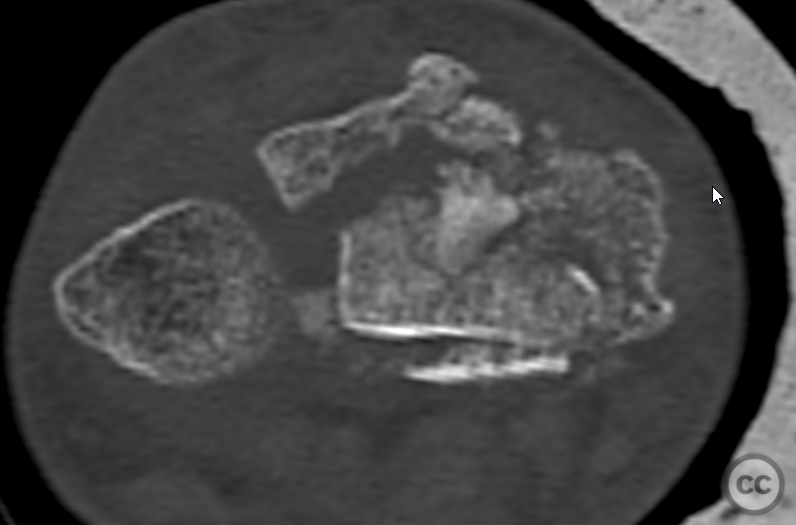
Articular die-punch Distal Radius Fracture with Dorsal Ulnar Corner Involvement
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: A 45-year-old male sustained a closed distal radius fracture after falling down stairs. The neurovascular examination was intact. Initial management included closed reduction and application of a plaster cast in the emergency department, with planned open reduction and internal fixation (ORIF) scheduled for five days post-injury.
Preoperative Plan
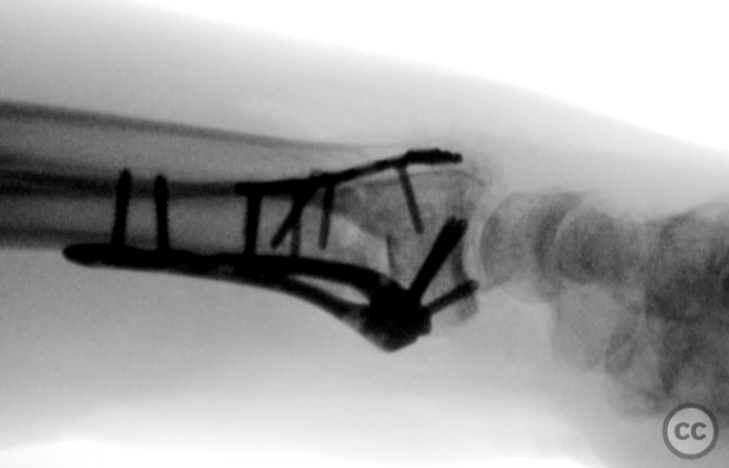
Planning remarks: The preoperative plan involved only a volar approach using a modified Henry incision to address the flipped die-punch fragment from the volar side. Things change, and intraoperatively, we limited the volar plan to securing the volar lip and processus styloideus radii with a volar plate, followed by a dorsal approach to address the dorsal ulnar corner and central articular fragments.
Surgical Discussion
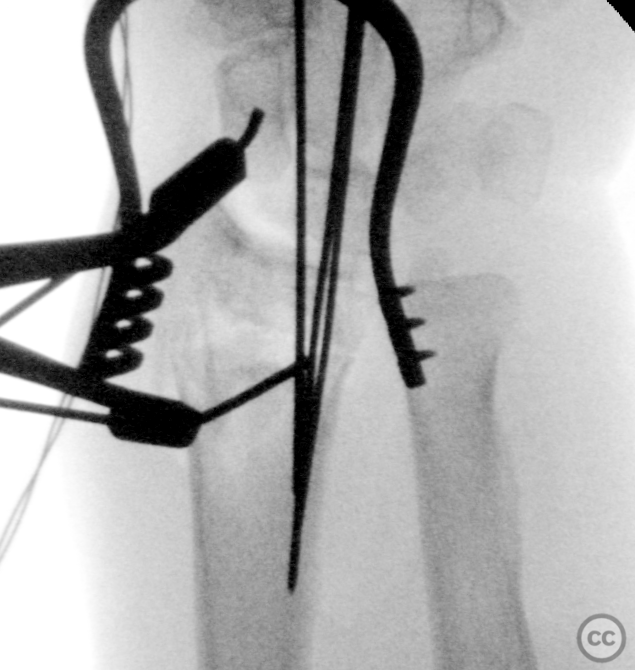
Patient positioning: The patient was positioned supine on a radiolucent operating table. The left arm was placed on an auxiliary arm table to facilitate access to the distal radius. A tourniquet was applied to the ipsilateral arm.
Anatomical surgical approach: A modified Henry approach was utilized, with a zigzag incision over the wrist. A separate dorsal incision over tuberculum Listeri into the 3rd extensor compartment allowed access to the dorsal ulnar corner.
Operative remarks:We utilised radiocarpal liamentotaxis over teh scaphoid and a k-wire distractor to allow gross reduction of teh articular geometry and restor radial inclincation against the proximal raction of brachioradialis. The die punch could not adequately be addressed from the volar fracture, thus the volar fixation was limited to securing the processus styloideus radii and volar lip. Dorsal exposure revealed a rupture at the base of the third compartment and displaced tuberculum Listeri fragment. Opening the dorsal cortex allowed identification of the die punch fragment which was manipulated and secured with a PLLA Drill-Pin. VITOSS bone void filler was used for further subchondral support. A mini-fragment T-plate provided anti-glide and buttress support for the dorsal ulnar corner.
Postoperative protocol: Postoperative rehabilitation included immobilization in a splint with gradual mobilization exercises initiated under supervision to restore range of motion and strength.
Follow up: Not specified
Orthopaedic implants used: Synthes two-column distal radius plate, Stryker mini-fragment system 2.0-millimeter lag screw, 2.0-millimeter mini-fragment T-plate, VITOSS bone void filler, 1.5-millimeter Arthrex PLLA Trim-It Drill-Pin
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisTechnical Analysis: Use of Dual Approach and BR Preservation
The described case utilized a sequential volar and dorsal approach. Initial plans for a volar-only reduction were revised intraoperatively, reflecting the frequent need for adaptability in addressing multi-fragmentary intra-articular fracture patterns. The authors describe the preservation of brachioradialis and its indirect role in maintaining radial inclination achieved via ligamentotaxis, rather than proceeding with BR tenotomy or release to facilitate reduction. This is a common decision point during distal radius fracture management, and the current literature provides insight into the risk and benefit profile of BR tenotomy.
Two comparative clinical studies (Ma et al. [1], Kim et al. [2]) have addressed the functional consequences of deliberate BR release. Both demonstrate that BR tenotomy, when performed during volar plate fixation for AO Type C fractures, enables improved fracture exposure and reduction without compromising elbow flexion strength or functional wrist outcomes in the early or mid-term period. Ma et al. further quantified reduced operative time with tenotomy, suggesting potential procedural gains. The present case did not report difficulties with BR tension obstructing reduction but documented reliance on external traction (k-wire distractor, ligamentotaxis). This is a viable approach, yet in similar fractures where satisfactory reduction cannot be attained, current evidence supports a low complication risk from BR release should it be deemed necessary.
Approach and Reduction of Dorsal Ulnar Corner
The necessity for additional dorsal exposure arose due to the inability to manipulate and secure centrally displaced die-punch fragments via the volar approach. Access to the dorsal ulnar corner, and subsequent buttress with a mini-fragment T-plate, aligns with established principles for fragment-specific fixation in complex articular injuries. The case also describes using a PLLA Drill-Pin for die-punch stabilization and bone void filler to address subchondral loss; while these interventions are supported in various small series and technical descriptions, their impact on mid- or long-term outcomes compared with alternatives (e.g., structural bone graft) remains under-investigated.
Hohendorff et al. [3] discuss the use of a portion of the BR insertion for repair of the pronator quadratus after volar plating, improving coverage and potentially reducing flexor tendon complications. The case report does not specify the handling of the pronator quadratus, nor flexor tendon protection measures, or addresses plate-related complications. The literature suggests consideration of these measures, especially with dual plating, which can increase the risk of soft tissue irritation.
Implant Selection and International Practice Variability
The hardware selection in this case (Synthes two-column plate, Stryker and Arthrex adjuncts) is within the range of contemporary, widely available systems in resource-rich settings. Use of biodegradable pins and synthetic bone void filler reflects evolving trends in biologic and hardware adjuncts but may have variable availability globally.
Critical Gaps
Despite a detailed operative description, documentation of postoperative course, timelines to union, and functional outcomes (range of motion, grip strength, return to work/ADLs, patient-reported outcomes) is lacking. The absence of follow-up data significantly limits assessment of success and comparability. Evidence from the reviewed literature highlights the importance of structured, time-based functional assessment to substantiate the safety and efficacy of complex interventions, especially in multifragmentary articular fractures.
No discussion is offered regarding the complications associated with dual plating (e.g., extensor tendon irritation/rupture from dorsal hardware), or assessment for potential alternative techniques that may limit dorsal exposure (such as volar-only plating with indirect reduction and supplementary fragment fixation).
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










User Discussion (1)
MED
Good results! Thanks for the Knowledge.