Complex Pelvic Ring Disruption with Bilateral SI, Bilateral Ramus, and Symphyseal Injuries in a Young Adult Female
Score and Comment on this Case
Clinical Details
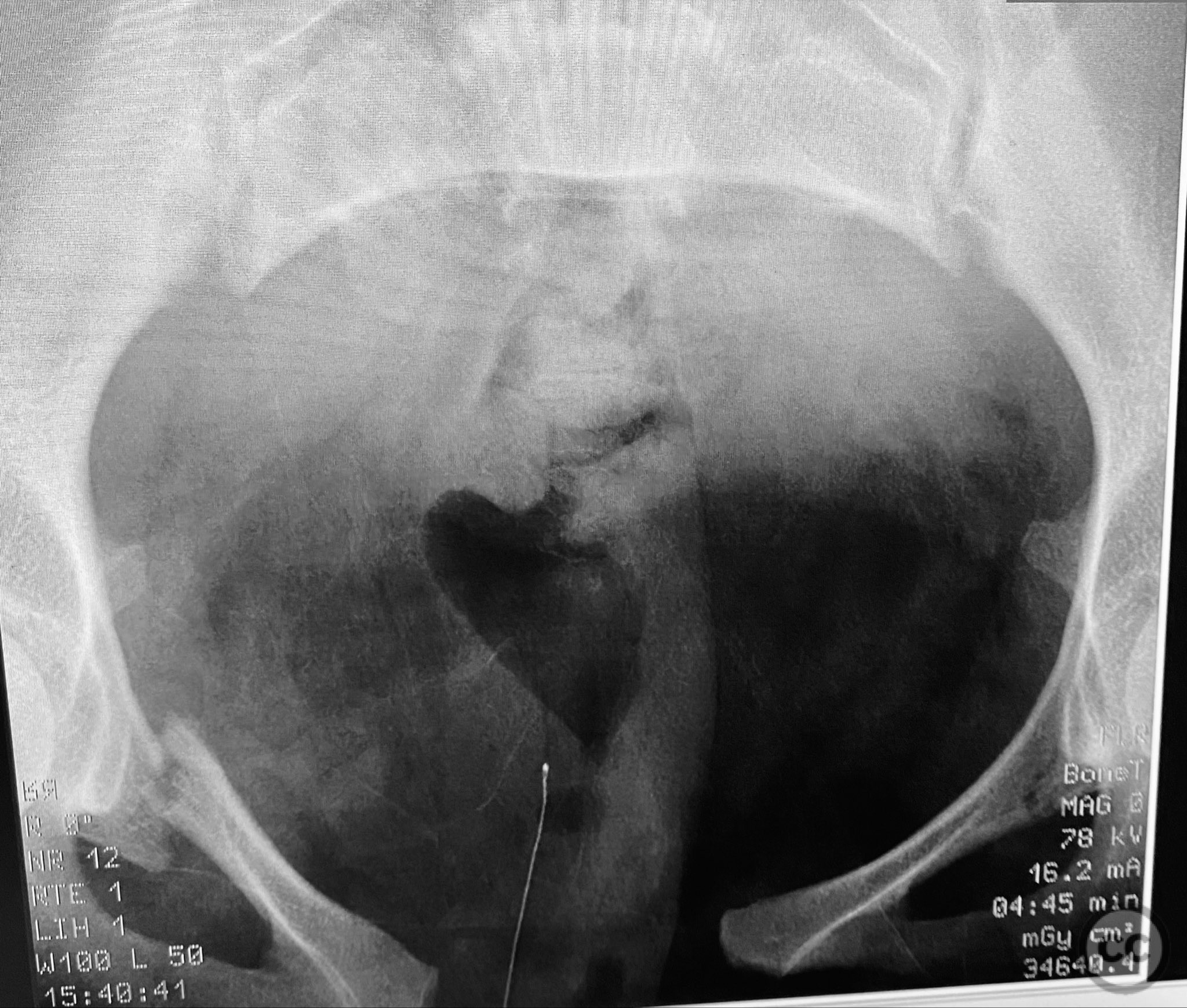
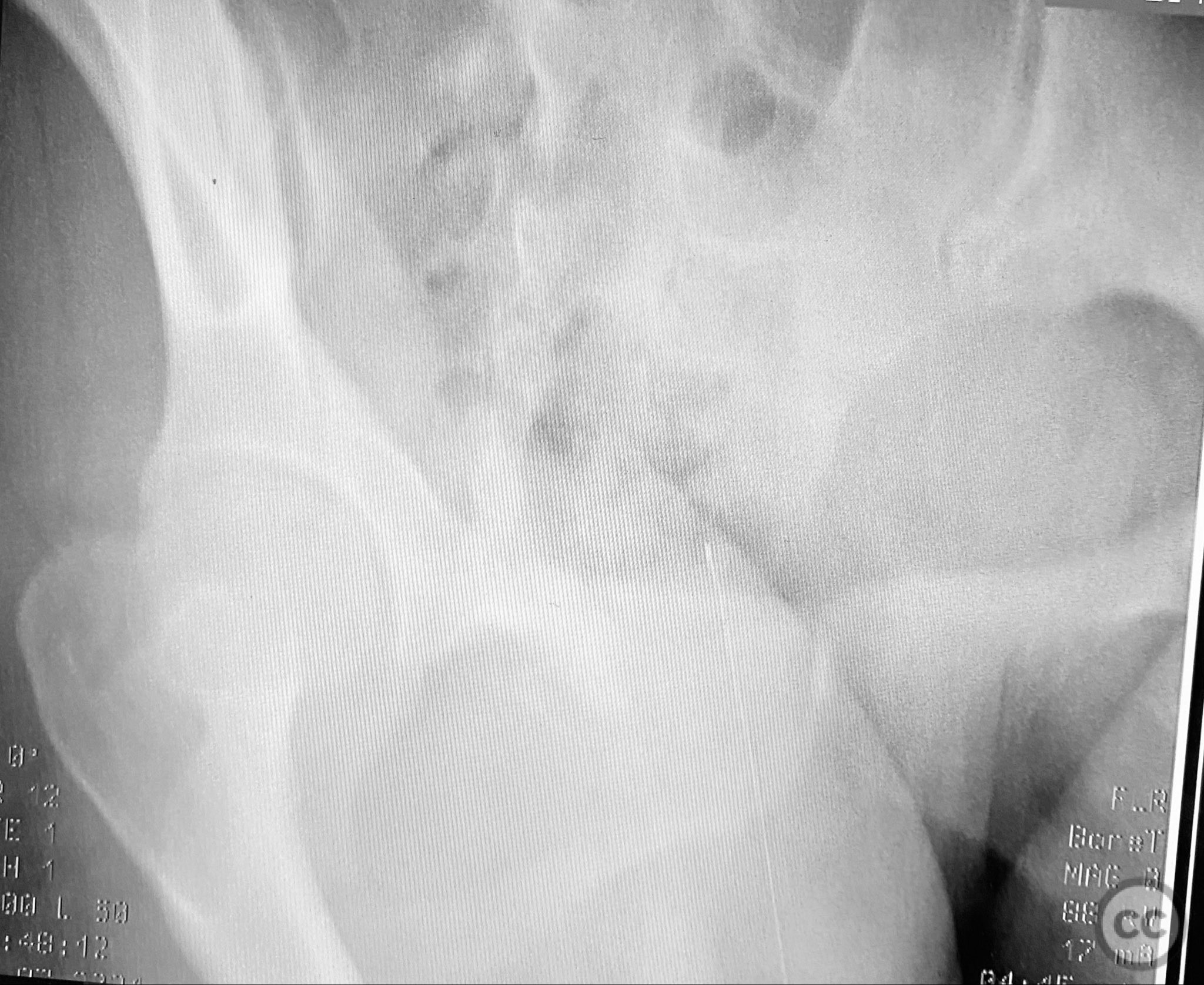
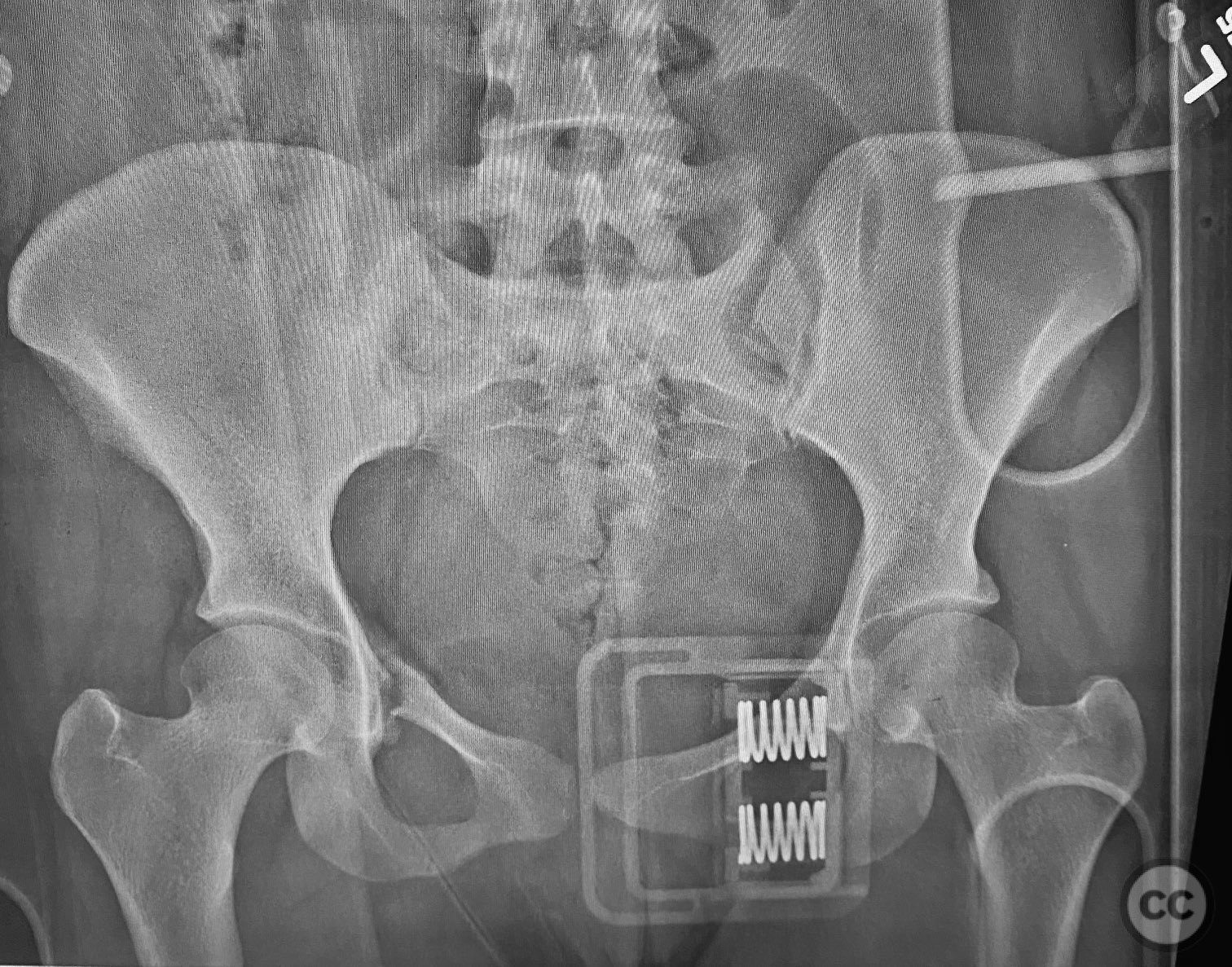
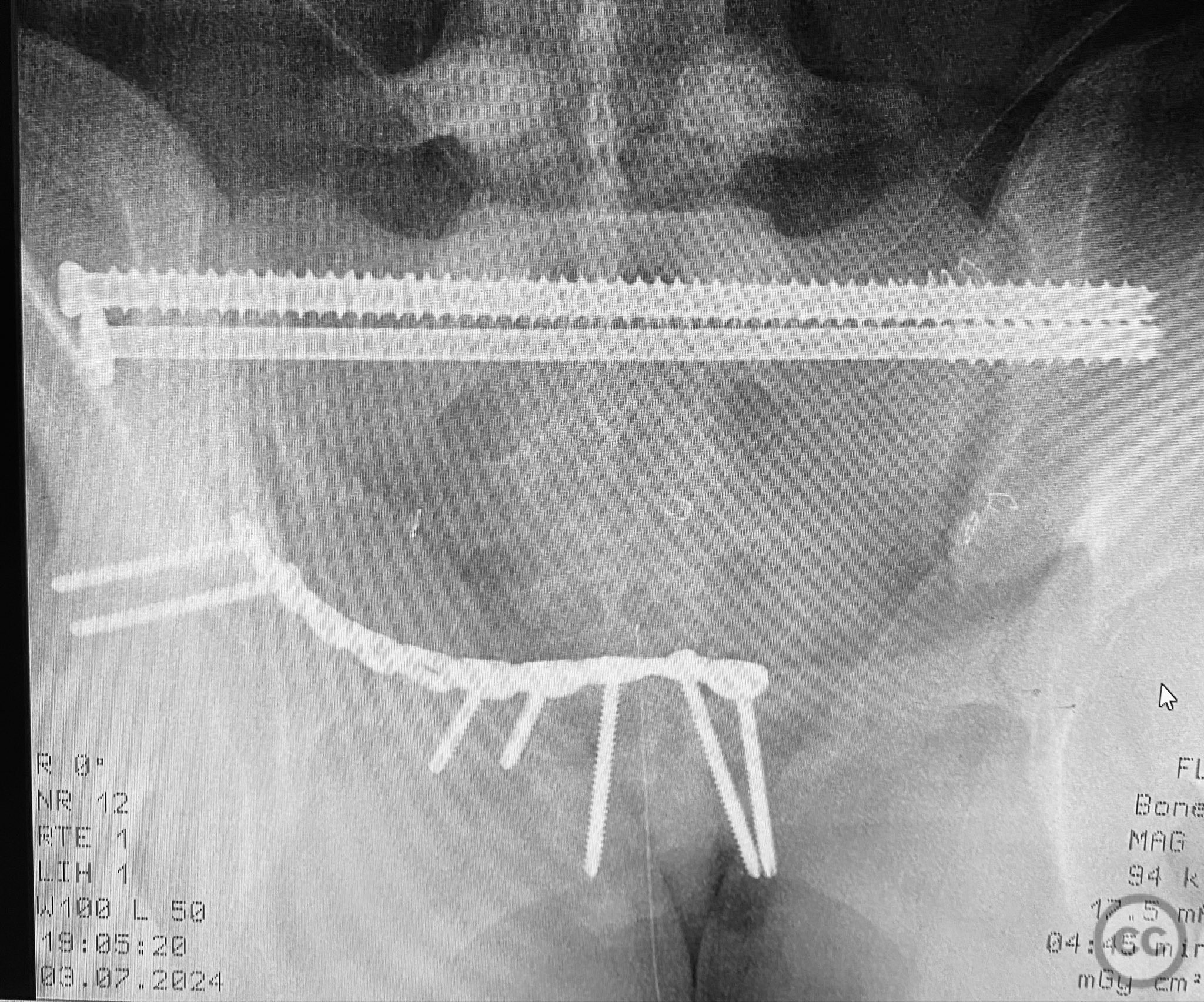
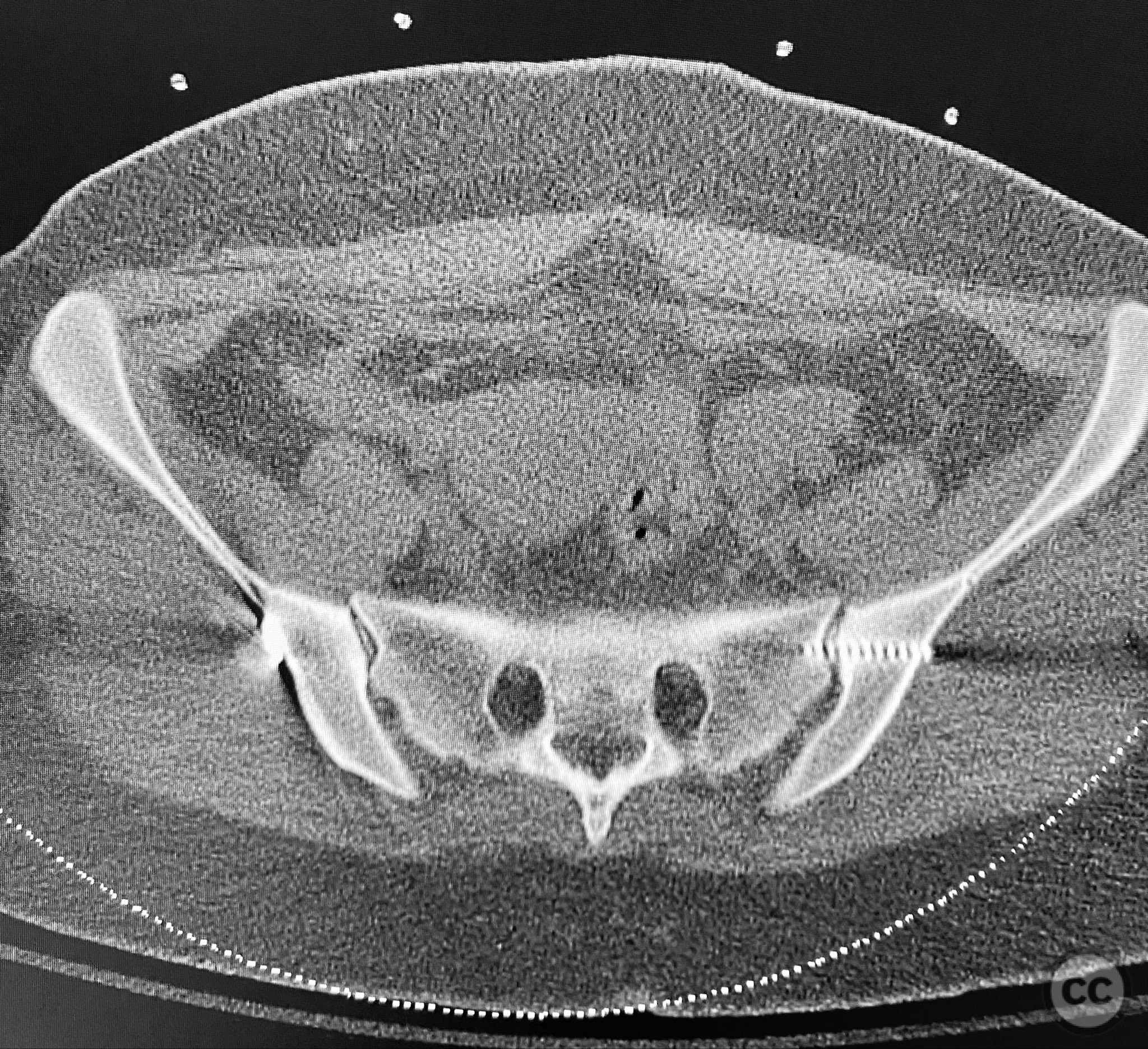
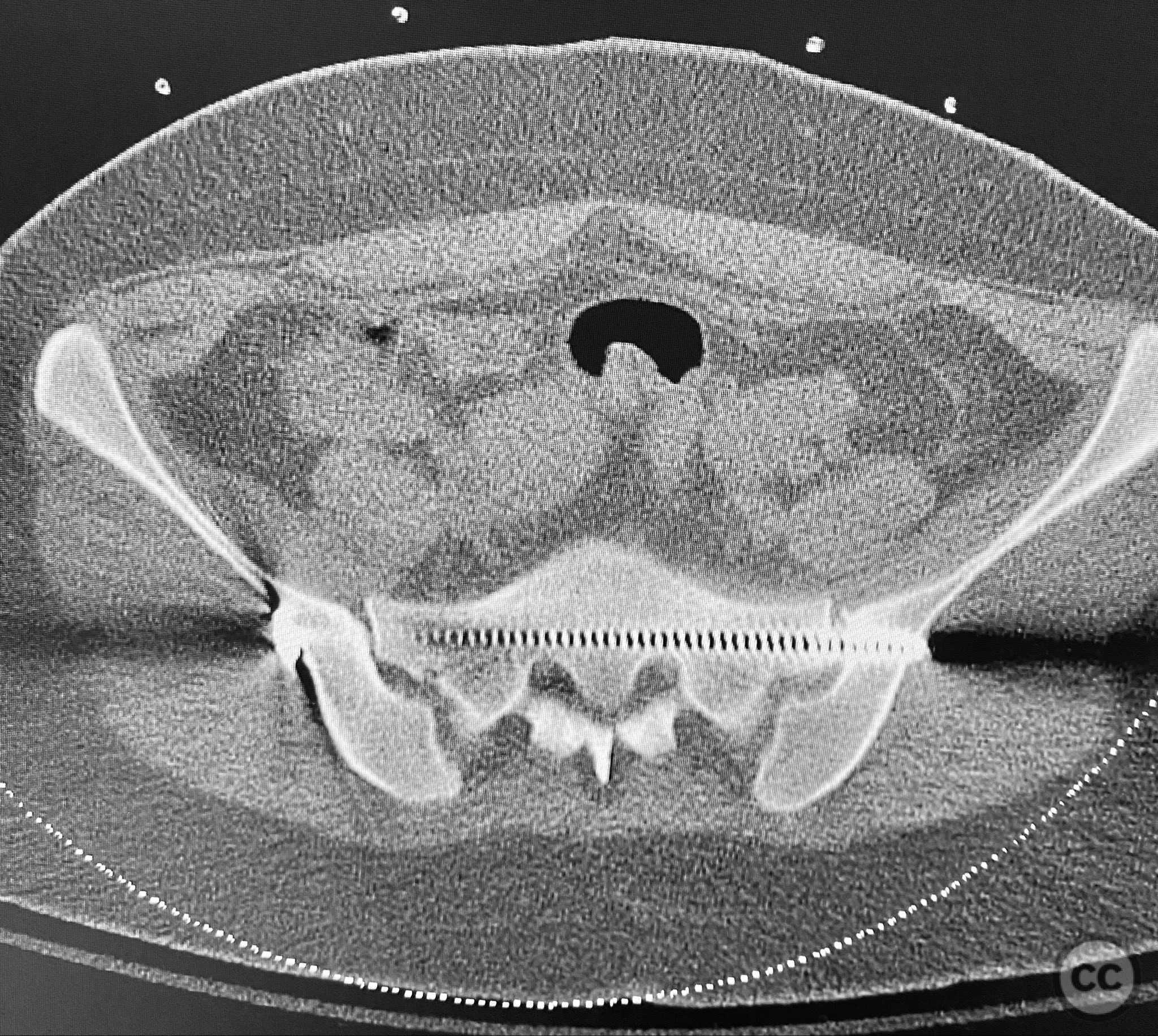
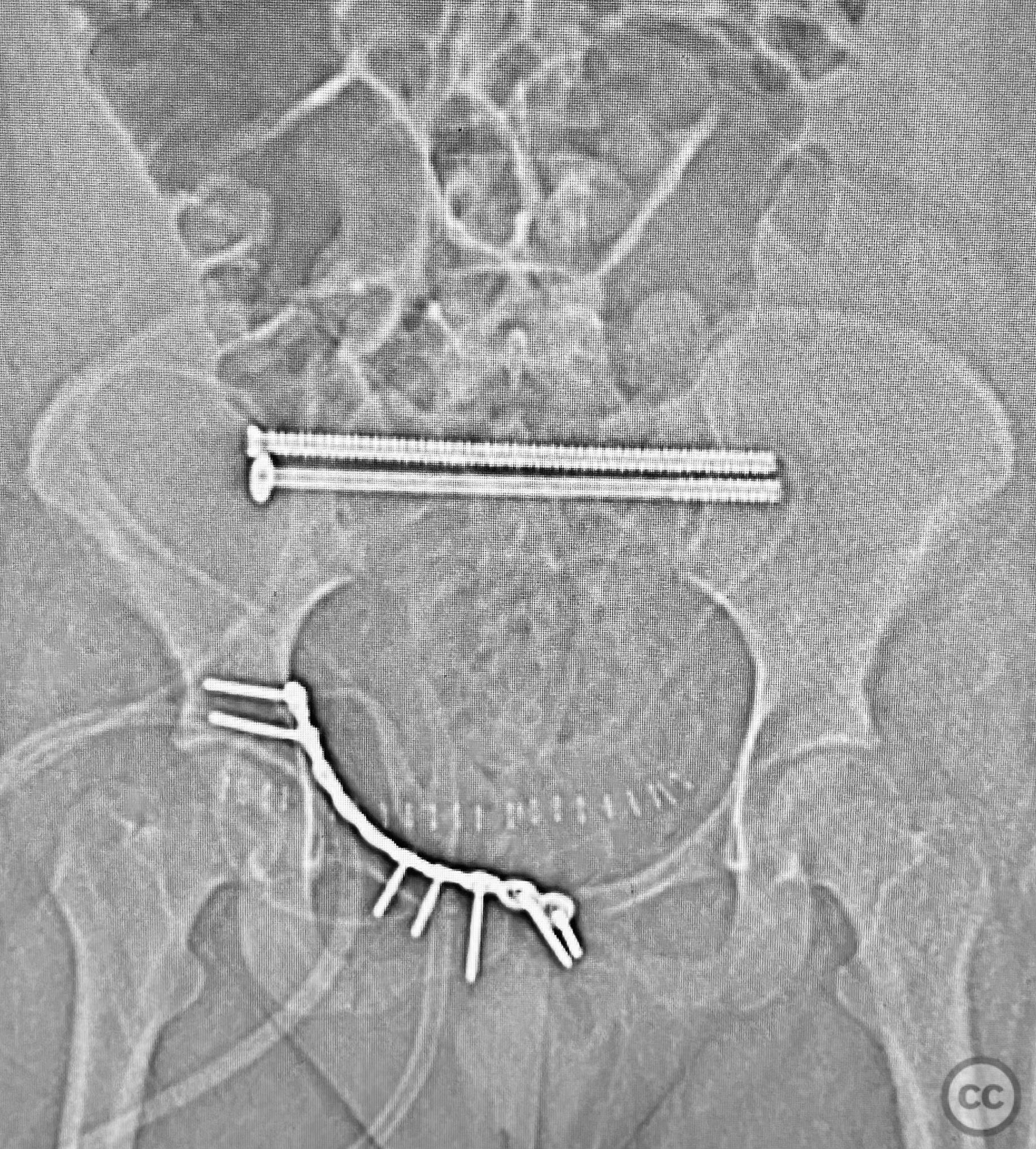
Clinical and radiological findings: A young adult female sustained a high-energy pelvic injury following a motorcycle crash. She was hemodynamically stable on presentation, with normal neurovascular examination and no evidence of genitourinary, vaginal, or rectal injury. She reported pain localized to both anterior and posterior pelvic regions. Initial plain radiographs (with and without pelvic binder) demonstrated multiple anterior ring fractures and dislocations. The binder images obscured the full extent of injury. Further intraoperative fluoroscopic imaging (AP, inlet, and with lower extremities in "lotus" position) revealed bilateral sacroiliac (SI) joint disruptions (right greater than left), bilateral superior/inferior pubic ramus fractures (right greater than left), and symphyseal diastasis. Notably, the right pubic ramus demonstrated excessive curvature, complicating potential percutaneous screw fixation. AO/OTA classification: 61-C1.3 (bilateral complete disruption of the posterior arch with associated anterior ring injury). Young-Burgess classification: APC III.
Preoperative Plan
Planning remarks: The preoperative plan included open reduction and internal fixation (ORIF) of the displaced right pubic ramus fracture and symphyseal diastasis via an anterior approach, with acceptance of indirect closed reduction of the SI joints. Percutaneous trans-sacral screw fixation was planned for stabilization of the posterior pelvic ring. Due to the complex curvature of the right ramus, straight screw fixation was deemed unsuitable.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent operating table under general anesthesia. For intraoperative assessment, the lower extremities were placed in a "lotus" position to enhance visualization of pelvic ring injuries under fluoroscopy.
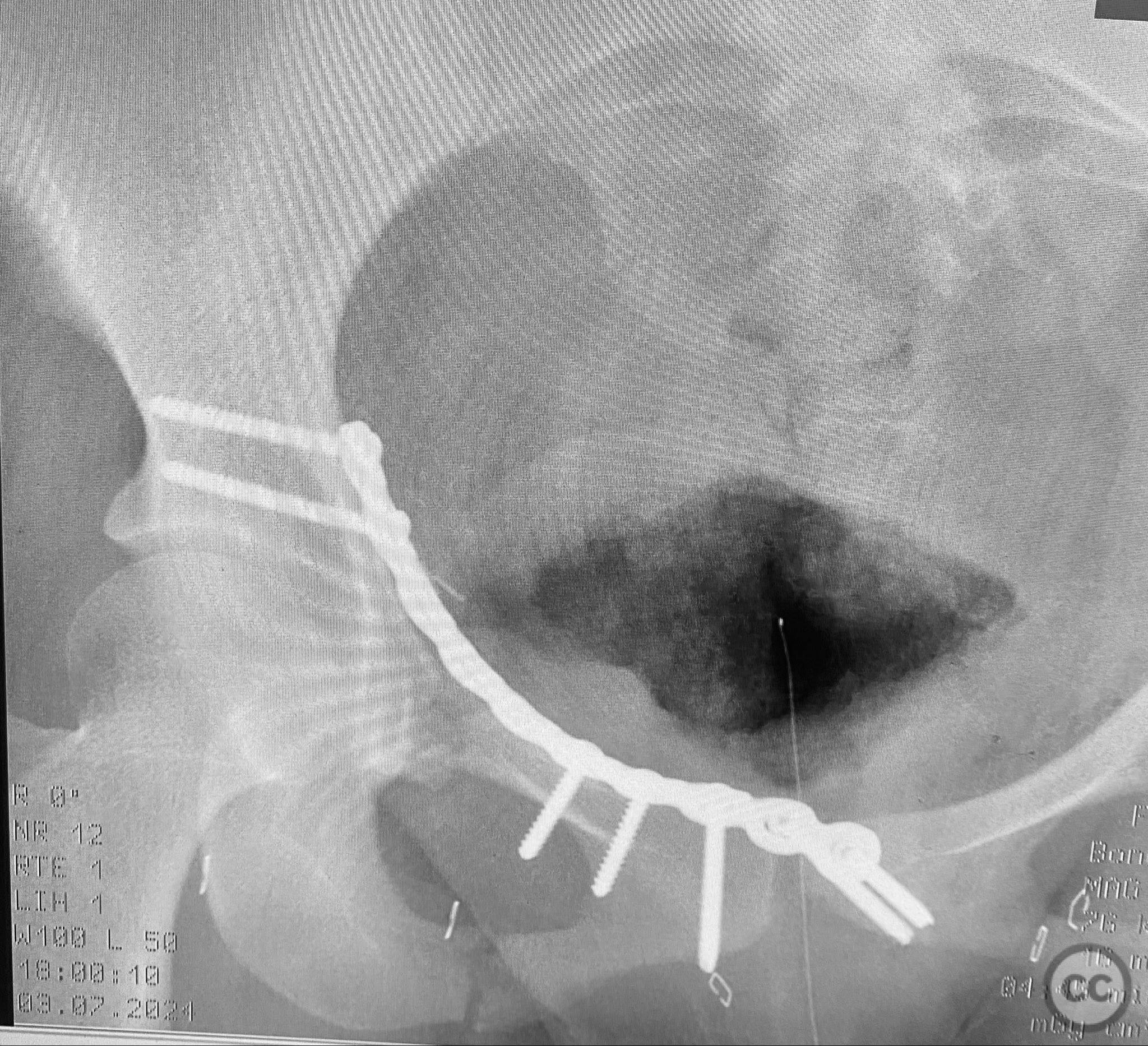
Anatomical surgical approach: A combined Pfannenstiel and intrapelvic (modified Stoppa) approach was utilized. A transverse suprapubic skin incision was made approximately two fingerbreadths above the symphysis pubis. Dissection proceeded through the subcutaneous tissue and rectus sheath, with careful subperiosteal elevation of the rectus abdominis from the anterior pelvic ring. The retropubic space (Cave of Retzius) was developed to expose the symphysis pubis and superior pubic rami bilaterally. Intrapelvic exposure allowed direct visualization and reduction of the displaced right pubic ramus fracture and symphyseal diastasis. A pre-contoured plate was applied to the anterior ring using both direct and indirect reduction techniques.
Operative remarks:Intraoperative fluoroscopy with AP and inlet views, as well as dynamic positioning of the lower extremities, was critical in fully delineating the extent of injury, which had been underestimated on preoperative imaging due to binder application. The excessively curved morphology of the right pubic ramus precluded safe or effective straight screw fixation; therefore, ORIF with a contoured plate was performed using intrapelvic exposure for optimal fit and stability. Indirect closed reduction of the SI joints was accepted, followed by percutaneous trans-sacral screw fixation under fluoroscopic guidance. This case highlights the necessity of thorough intraoperative assessment for occult or underestimated injury patterns in complex pelvic trauma, particularly when initial imaging is performed with a pelvic binder in situ.
Postoperative protocol: Early mobilization with protected weight bearing as tolerated using crutches or walker for 8–12 weeks. Thromboprophylaxis initiated postoperatively. Hip and knee range-of-motion exercises commenced on postoperative day one. Progression to full weight bearing guided by radiographic evidence of healing at 10–12 weeks.
Follow up: Not specified
Orthopaedic implants used: Pre-contoured anterior pelvic reconstruction plate; percutaneous trans-sacral cannulated screws
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities


.jpg)

Article viewed 141 times
11 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Complex Pelvic Ring Disruption with Bilateral SI, Bilateral Ramus, and Symphyseal Injuries in a Young Adult Female. Journal of Orthopaedic Surgery and Traumatology. Case Report 1257765 Published Online Sep 11 2025.