Complex Acetabular Posterior Wall and Transverse Fracture with Articular Impaction
Score and Comment on this Case
Clinical Details
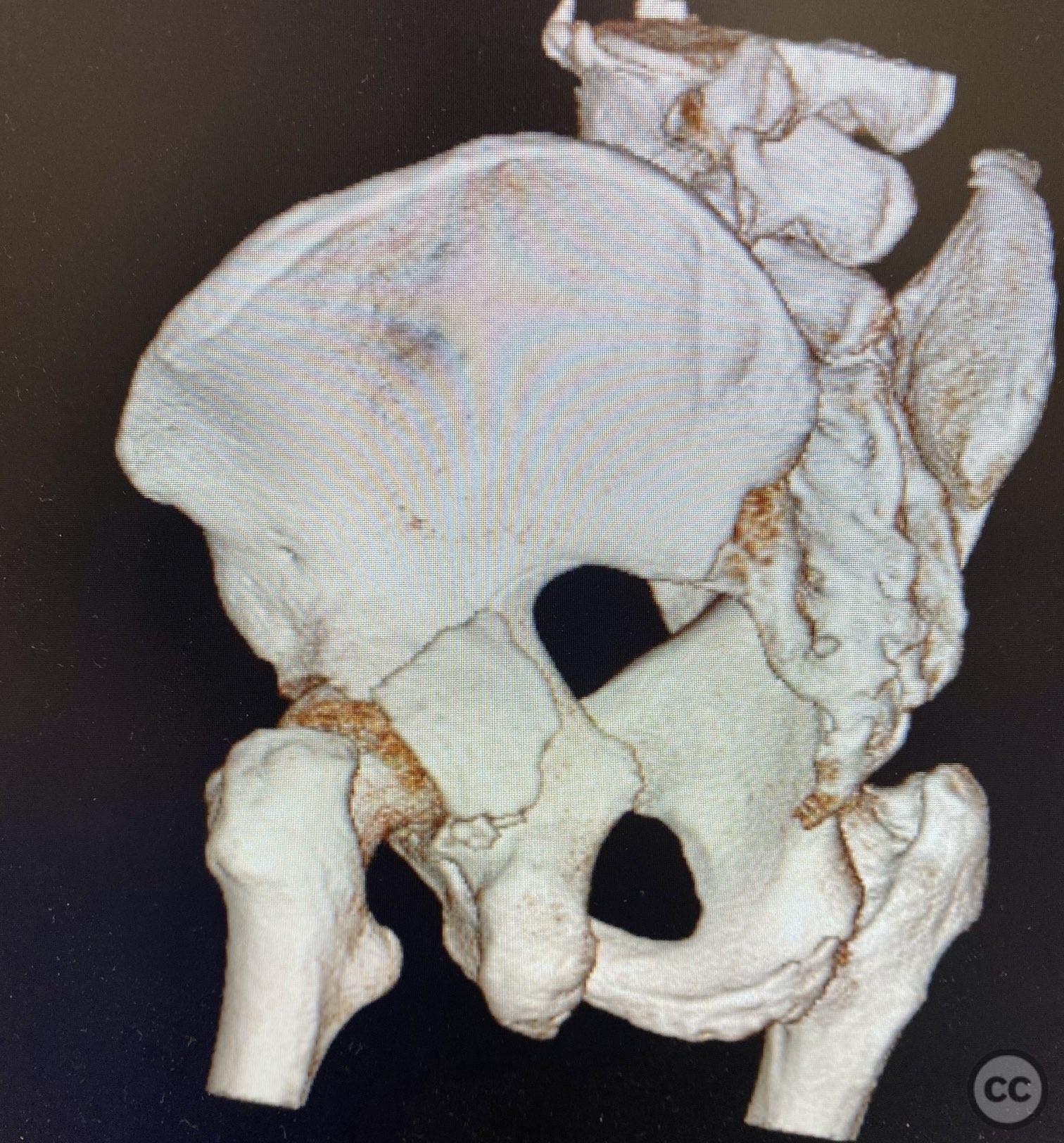
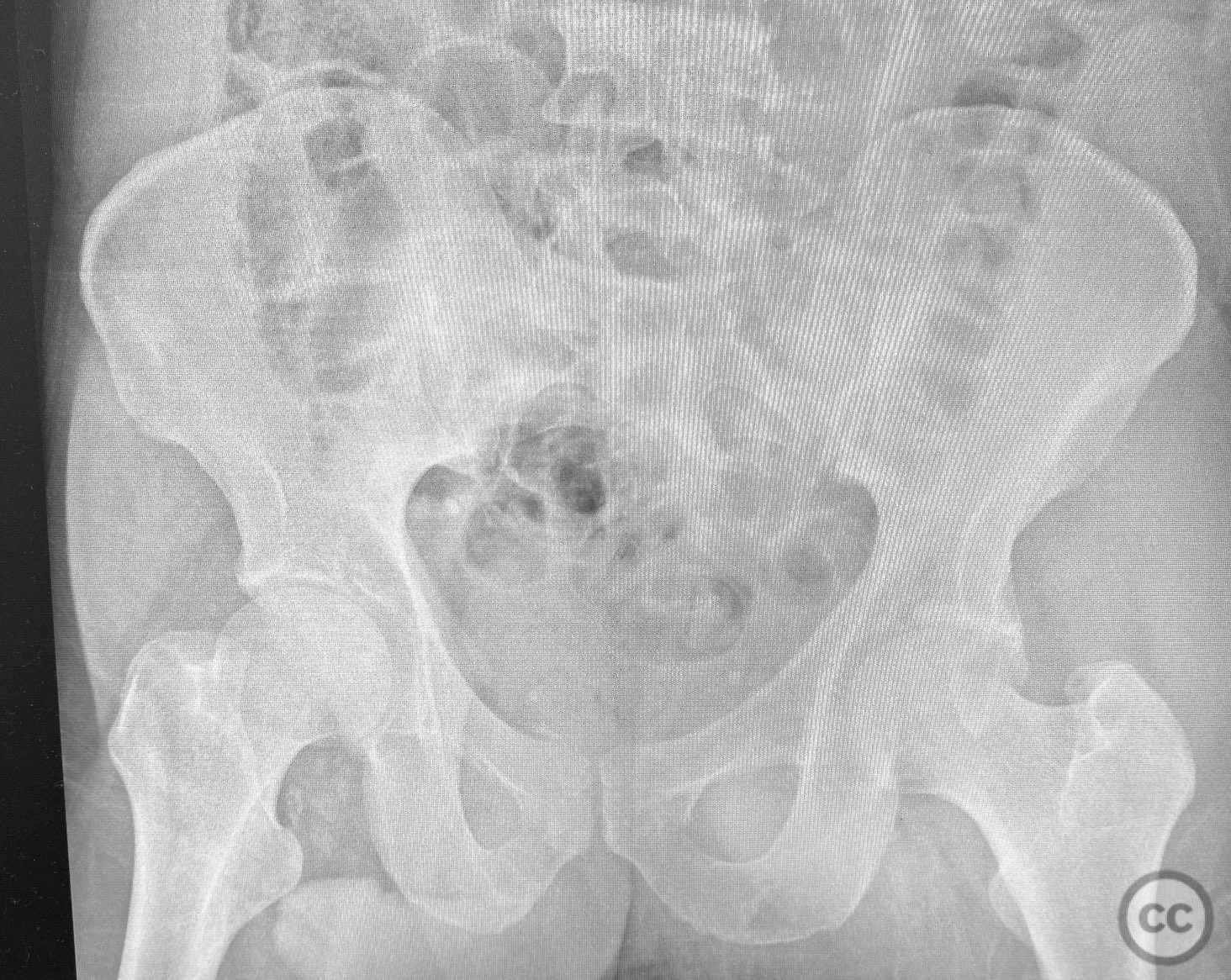
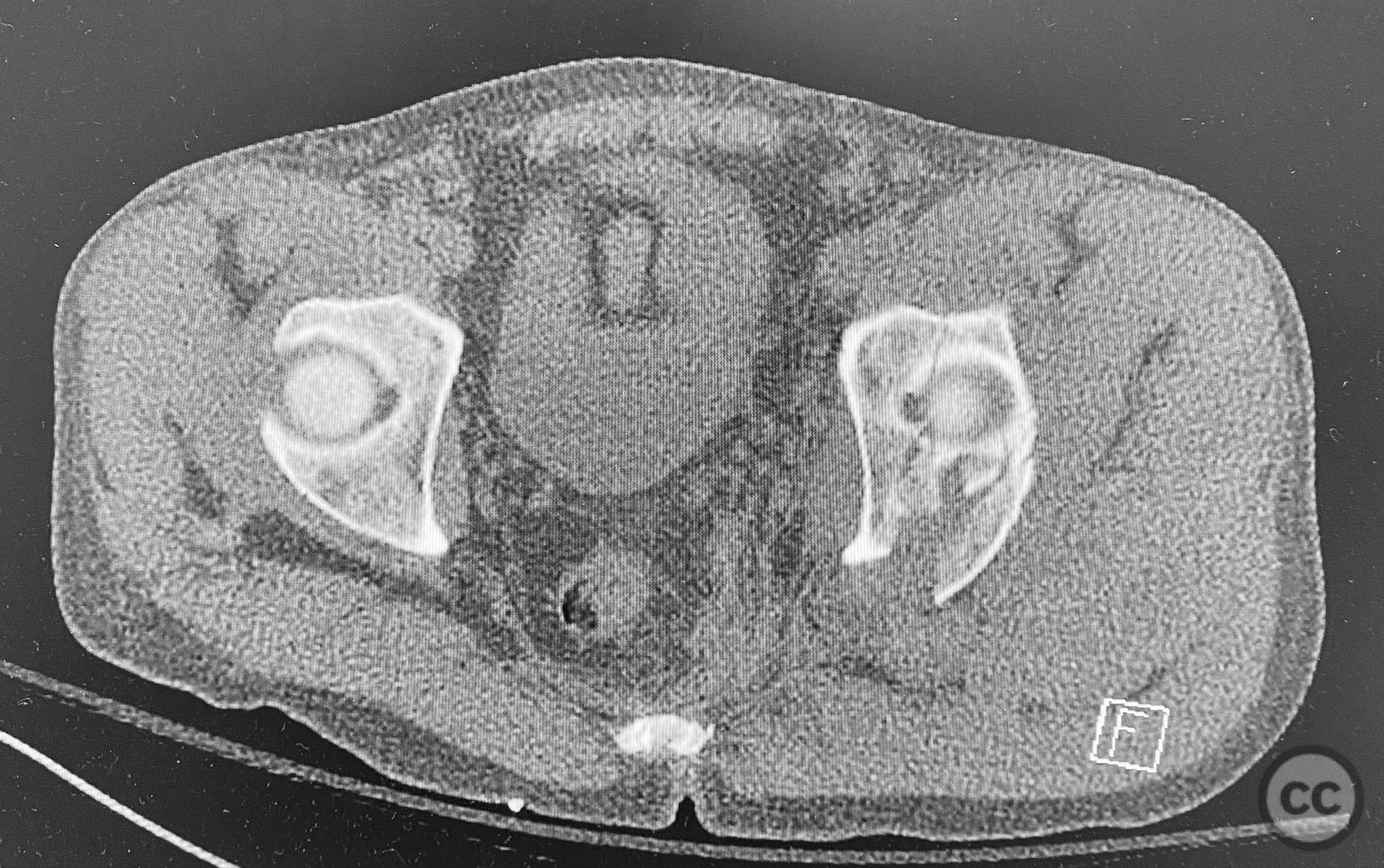
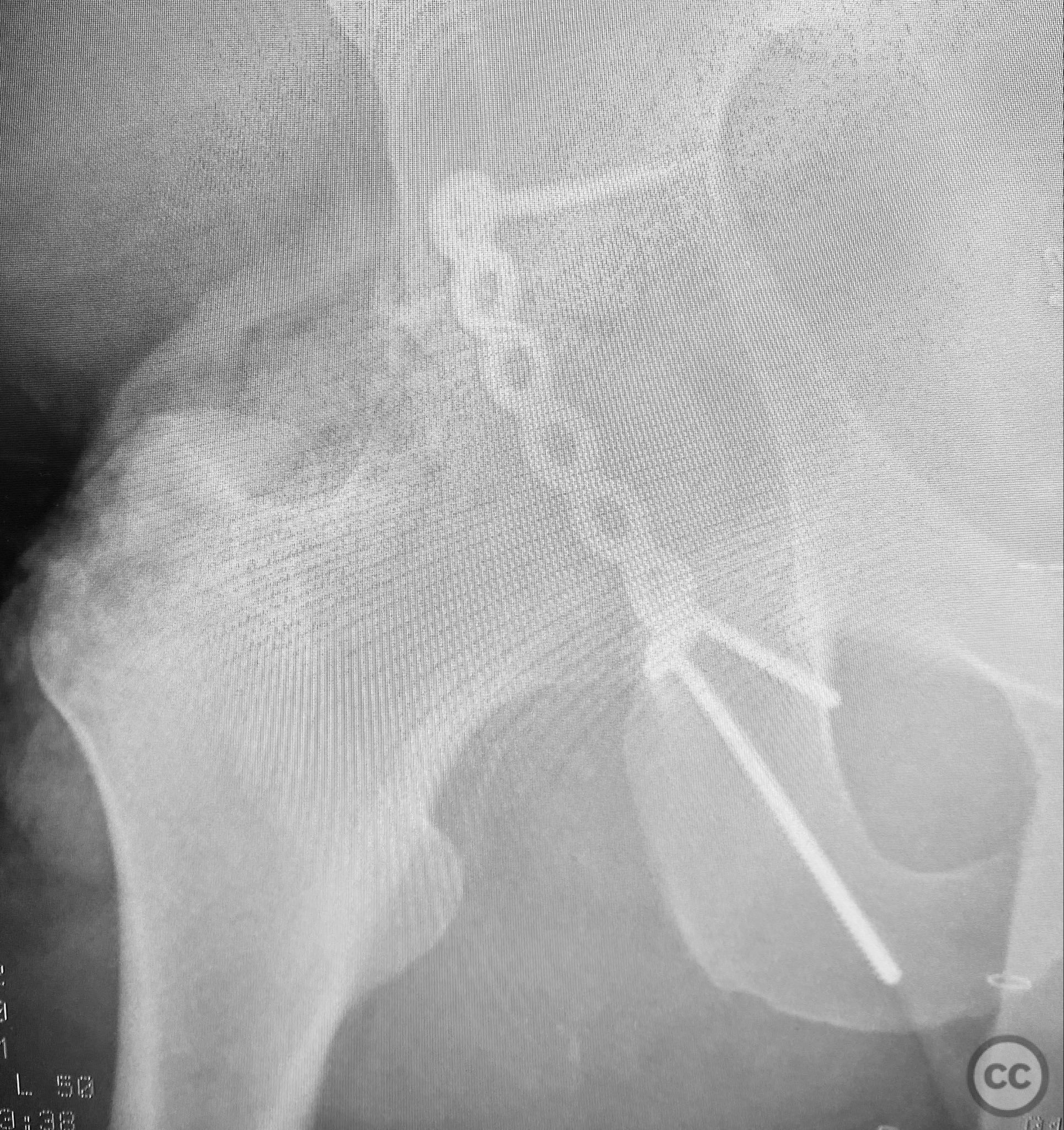
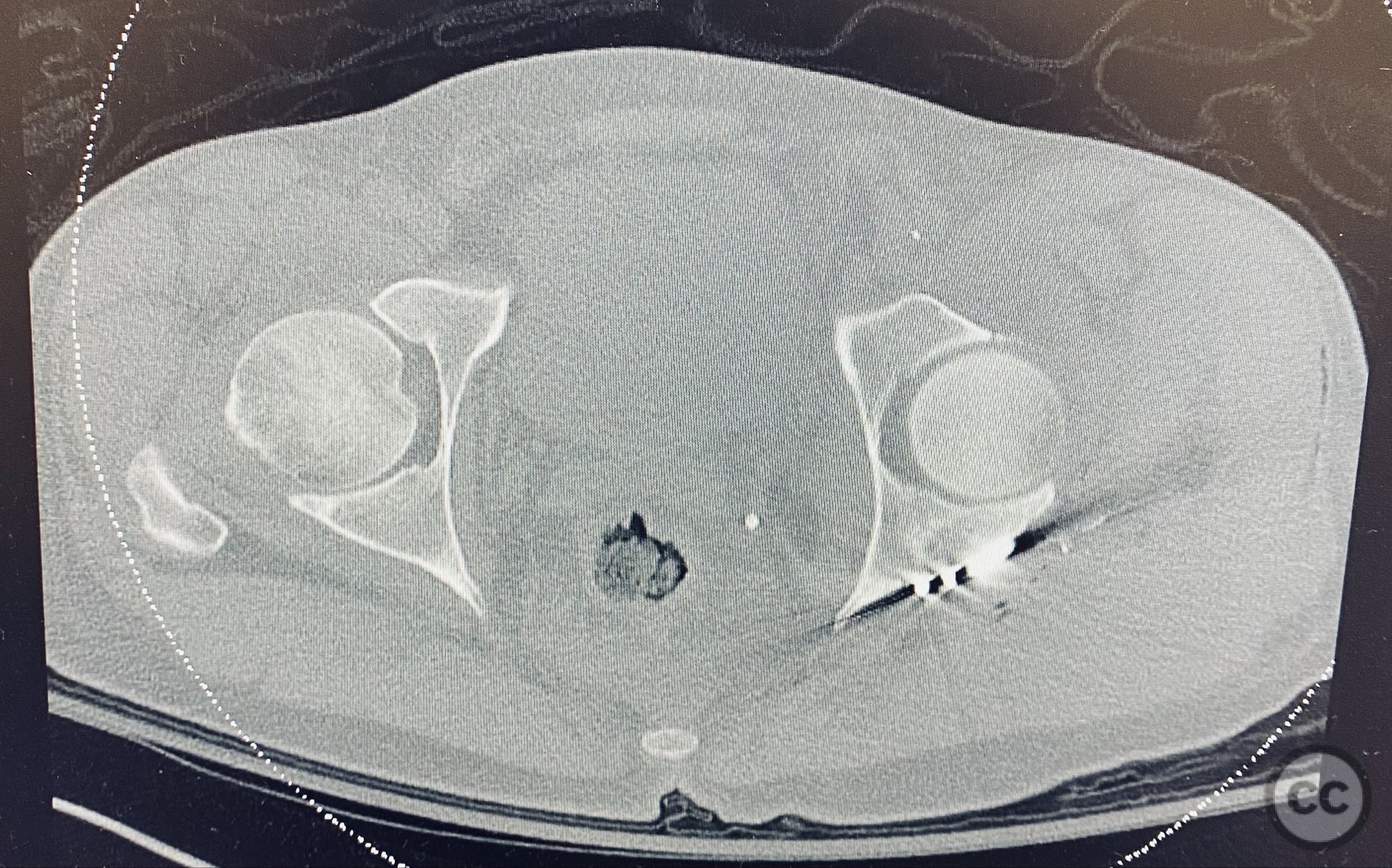
Clinical and radiological findings: A patient presented with a seemingly non-comminuted, wide, and long posterior wall (PW) acetabular fracture fragment. Axial computed tomography (CT) images demonstrated the thickness of the PW fragment, the articular surface, and multiple areas of subchondral impaction. Preoperative planning identified the size, location, and depth of the impaction zones, as well as an essentially nondisplaced transverse acetabular fracture line, which was not readily apparent on initial imaging. No significant displacement of the transverse component was noted. The AO/OTA classification is 62-B1.3 (posterior wall and transverse acetabular fracture).
Preoperative Plan
Planning remarks: The preoperative technical plan included a prone Kocher-Langenbeck (KL) approach to access the posterior column and wall. The plan entailed elevation and reduction of impacted articular fragments, bone grafting of subchondral defects, anatomical reduction and provisional fixation of the posterior wall fragment, and definitive fixation with a contoured plate. Intraoperative fluoroscopy was planned to guide additional screw placement through the plate to stabilize both the posterior wall and the transverse fracture line. A supplementary medial plate was planned to augment fixation of both the posterior wall and transverse components.
Surgical Discussion
Patient positioning: The patient was positioned prone on a radiolucent table to facilitate posterior pelvic access and intraoperative fluoroscopic imaging.
Anatomical surgical approach: A standard Kocher-Langenbeck approach was performed with a longitudinal incision centered over the greater trochanter, extending proximally along the gluteal region. The fascia lata was incised in line with the skin incision, and the gluteus maximus was split in the direction of its fibers. The short external rotators were identified, tagged, and released from their femoral insertions to expose the posterior column and wall of the acetabulum. The sciatic nerve was identified and protected throughout the procedure. The hip was distracted to visualize the dome; however, the transverse fracture line was not visible on direct inspection or on the cortical surface.
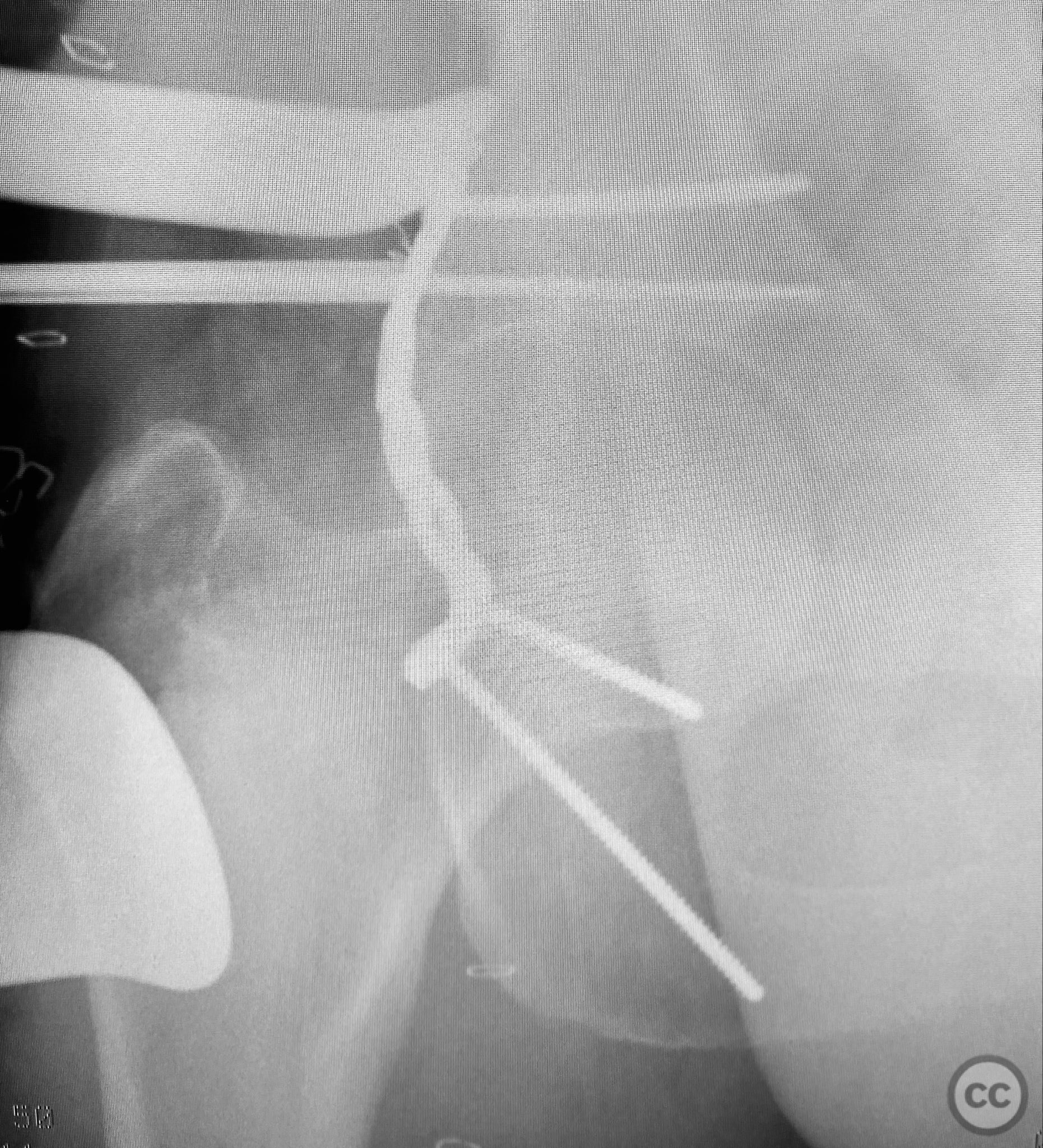
Operative remarks:Intraoperatively, elevation and reduction of impacted articular fragments were performed, followed by bone grafting of subchondral defects. The posterior wall fragment was anatomically reduced and initially stabilized with a contoured plate. Intraoperative fluoroscopy (obturator oblique view) was utilized to guide placement of an additional screw through the plate above the joint, traversing both the posterior wall fragment and stabilizing the transverse fracture line. A supplementary medial plate was applied to further support both fracture components. Postoperative CT imaging confirmed satisfactory reduction of both the posterior wall and transverse fractures, as well as restoration of articular congruity in previously impacted areas. Consideration is given to whether initial reduction and lag screw fixation of the transverse component prior to plate application may have improved reduction; however, final imaging demonstrated acceptable alignment.
Postoperative protocol: Early passive range of motion exercises were initiated postoperatively with toe-touch weight bearing for 8 weeks. Progressive weight bearing was allowed thereafter based on radiographic evidence of healing.
Follow up: Not specified
Orthopaedic implants used: 3.5 mm pelvic reconstruction plates (posterior wall and medial), 3.5 mm cortical screws, autologous bone graft
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities










Article viewed 465 times
12 Sep 2025
Add to Bookmarks
Full Citation
Cite this article:
Routt, ML. (2025). Complex Acetabular Posterior Wall and Transverse Fracture with Articular Impaction. Journal of Orthopaedic Surgery and Traumatology. Case Report 12030777 Published Online Sep 12 2025.