Proximal Tibia Nonunion with Varus Deformity Correction and Stabilization
Score and Comment on this Case
Clinical Details
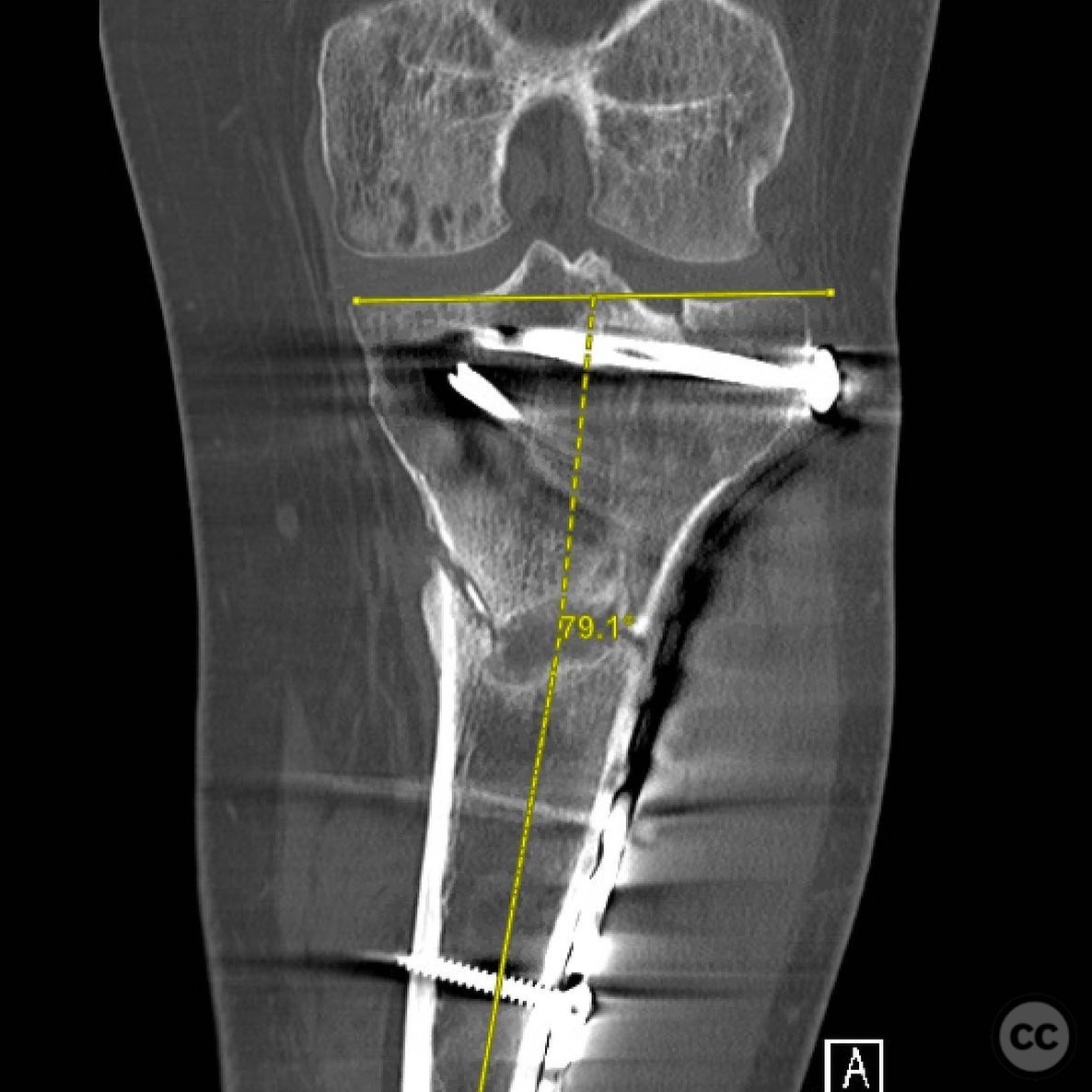
Clinical and radiological findings: A 30-year-old male, weighing 275 pounds, presented with a nonunion of the proximal tibia following a motocross accident. The initial injury was a closed fracture treated at an outside facility. Eight months post-injury, the patient reported persistent pain exacerbated by activity, inability to run or lift, and difficulty walking without pain. Radiological assessment revealed a varus deformity due to fatigue of a laterally based locking plate, which was insufficient for the patient's muscular build and resulted in inadequate medial load sharing.
Preoperative Plan
Planning remarks: The preoperative plan involved sequential correction of the coronal plane deformity, compression of the nonunion site, and stable fixation. The approach included removal of distal screws from the lateral plate, use of a medial distractor, lateral articulated tension device (ATD), fibular osteotomy, percutaneous osteoclasis through the nonunion site, and subsequent steps to achieve deformity correction and compression.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table to facilitate access to both medial and lateral aspects of the proximal tibia.
Anatomical surgical approach: A combined approach was utilized: initially addressing the lateral aspect through removal of distal screws from the existing plate, followed by a mini-open medial approach for buttress plating. Percutaneous osteoclasis was performed through the nonunion site to aid in deformity correction and stimulate healing.
Operative remarks:The surgeon noted that the primary issue was mechanical rather than biological, with the initial implant strategy being suboptimal for the patient's build. A lateral plate alone was insufficient due to lack of medial load sharing, leading to fatigue and varus deformity. Sequential correction techniques were employed, including distraction and compression methods, followed by stabilization with a nail and medial buttress plating. The intra-articular malunion was deemed irrelevant to the patient's outcome, and precise correction without over-correction into valgus was prioritized.
Postoperative protocol: Postoperative rehabilitation included weight-bearing as tolerated with gradual progression based on pain and stability. Emphasis was placed on maintaining alignment and encouraging early mobilization to promote healing.
Follow up: Not specified
Orthopaedic implants used: Lateral locking plate, medial buttress plate, intramedullary nail, bicortical screw, articulated tension device (ATD).
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities
















Article viewed 178 times
13 Jul 2025
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2025). Proximal Tibia Nonunion with Varus Deformity Correction and Stabilization. Journal of Orthopaedic Surgery and Traumatology. Case Report 11642720 Published Online Jul 13 2025.